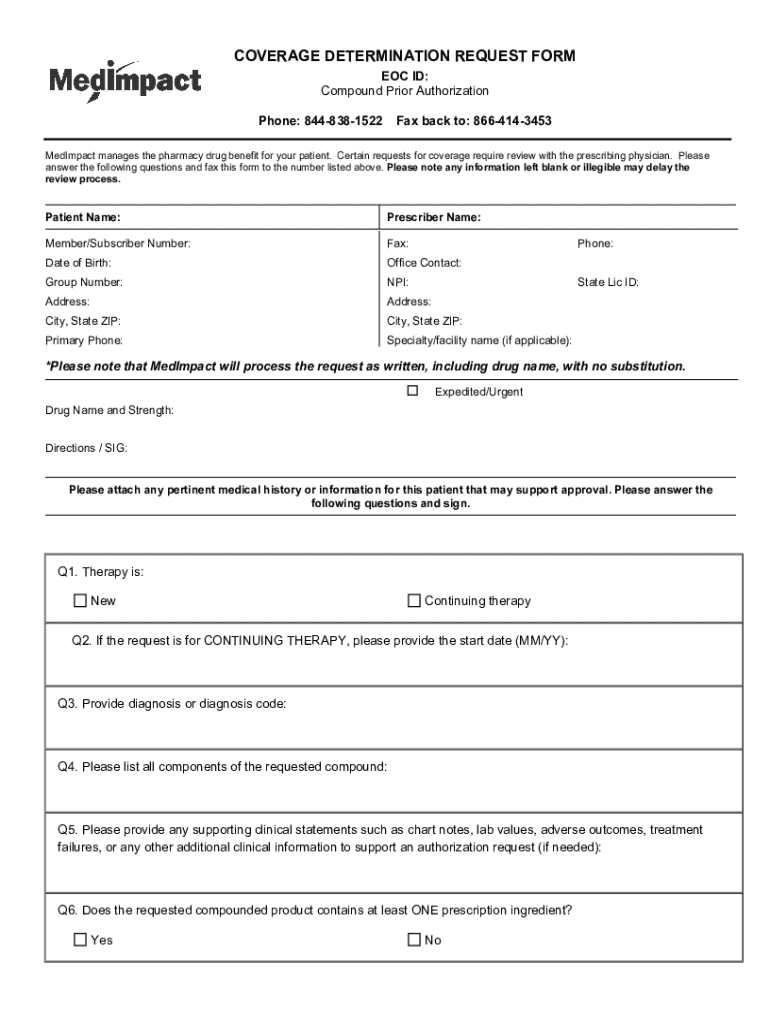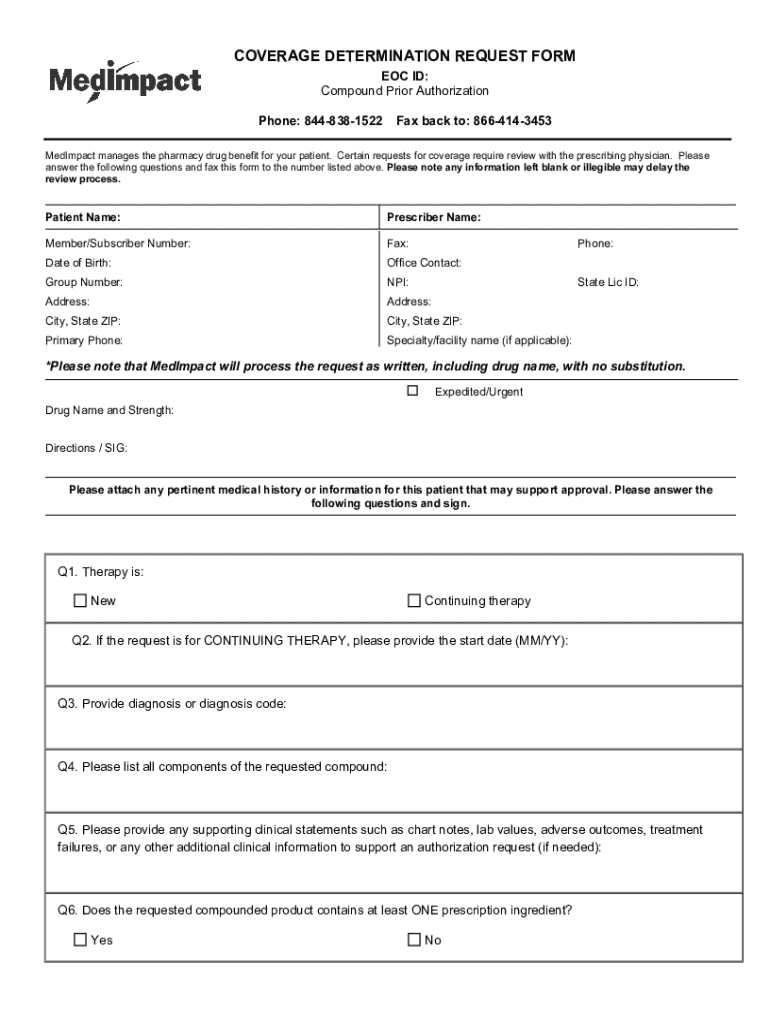
Get the free Coverage Determination Request Form
Get, Create, Make and Sign coverage determination request form
Editing coverage determination request form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out coverage determination request form
How to fill out coverage determination request form
Who needs coverage determination request form?
Coverage Determination Request Form - Your Comprehensive How-to Guide
Understanding the coverage determination request form
A coverage determination request form is a crucial document used in the healthcare sector, primarily to seek approval from insurance providers for specific medical services or prescriptions. This form serves as a formal request to determine whether a particular service, medication, or treatment is covered under a patient’s health insurance plan. The process is vital for patients who may require treatments not explicitly included in their insurance plan’s standard coverage.
Navigating the complexities of modern healthcare can be daunting. The coverage determination request form plays a significant role in unlocking necessary healthcare services. When patients are faced with new treatments or medications, this request ensures that they can access their needed care without overwhelming financial burden.
When is a coverage determination request needed?
Coverage determination requests are often needed in various scenarios, including when a patient requires a specific type of medication not listed on their formulary, or when a proposed treatment is deemed experimental or not typically covered by the insurance plan. Additional situations can arise when changes in a patient's health necessitate new treatments or specifications, thus prompting the need for this form.
Navigating the coverage determination process
Before submitting a coverage determination request form, it’s essential to understand the eligibility criteria. Generally, the patient or their healthcare provider can file the request, although some insurance policies may have specific conditions that need to be met. For instance, prior authorization might be required under certain circumstances, especially for high-cost treatments.
Key terminology is often encountered throughout this process, necessitating familiarity with terms such as 'prior authorization', 'formulary', and 'denial'. Having a clear understanding of these concepts assists in crafting a well-structured request and determining its collective success.
Step-by-step instructions for completing the form
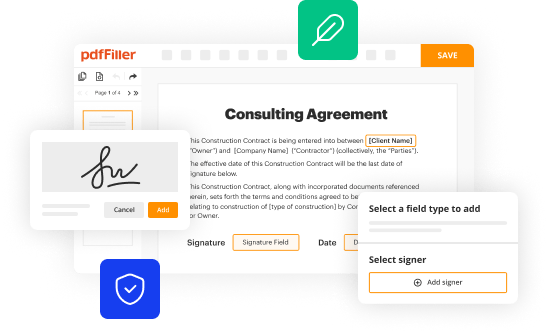
Completing the coverage determination request form accurately is imperative for successful submissions. Start by gathering necessary information, including patient details, the specific treatment or medication requested, and a justification of medical necessity. Having these details at hand will reduce delays in processing.
When filling out the form, it’s essential to pay close attention to each section. Ensure that the patient’s information, healthcare provider’s details, and the requested services or medications are filled out thoroughly. One key element is to include substantial medical justification, which shows the insurance company why the treatment is necessary for the patient's health. Missing or unclear information can lead to delays or denials.
Submitting the coverage determination request
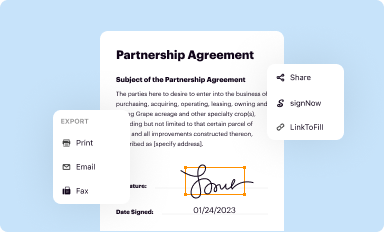
Once the coverage determination request form is completed, it’s time to submit it. Various channels exist for submission, including online submission through platforms like pdfFiller, faxing the document, or mailing it. Each option has its nuances, and understanding the most efficient way to submit according to the specific insurance provider can save time and hassle.
It is also crucial to be aware of submission timelines. Processing times can vary significantly across insurance providers, but generally, you can expect a response within a few days to a couple of weeks. Post-submission, maintain open lines of communication to track the status of your request.
Tracking your request
After submitting the coverage determination request form, utilizing tracking tools can ease the anxiety of waiting. pdfFiller provides users with specific features that allow them to monitor the status of their requests effectively. Set reminders in case follow-ups are needed, ensuring that no delays go unanswered.
When it comes time to follow up with insurers or providers, be prepared with relevant information. Clear records of your submission dates, reference numbers, and the specific details of the request will streamline the communication process and increase the chances of obtaining the necessary information swiftly.
Handling denials and appeals
There are times when a coverage determination request may be denied. Understanding why denials occur is essential for addressing them effectively. Common reasons include lack of medical necessity, services deemed experimental, or failing to follow the specific process set forth by the insurer.
If a denial is received, it’s crucial to act quickly. Gathering supporting evidence, such as additional medical records or a letter of medical necessity from the healthcare provider, will strengthen your case when appealing. Re-filing the request with revised justifications also increases the chance of obtaining approval.
Best practices for using the coverage determination request form
To ensure a smooth process when using the coverage determination request form, following best practices is essential. Keeping your documentation organized, accurate, and ready to go will speed up both the initial request and any subsequent appeals. Collaboration features available on pdfFiller can also enhance teamwork in filling out submissions.
Staying updated with changes in coverage policies is another best practice. Insurers frequently revise their terms and conditions, so accessing reliable resources and keeping abreast of updates will give you an advantage when dealing with requests.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I manage my coverage determination request form directly from Gmail?
Where do I find coverage determination request form?
Can I create an electronic signature for the coverage determination request form in Chrome?
What is coverage determination request form?
Who is required to file coverage determination request form?
How to fill out coverage determination request form?
What is the purpose of coverage determination request form?
What information must be reported on coverage determination request form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.