Get the free Michigan Prior Authorization Request Form
Get, Create, Make and Sign michigan prior authorization request
Editing michigan prior authorization request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out michigan prior authorization request
How to fill out michigan prior authorization request
Who needs michigan prior authorization request?
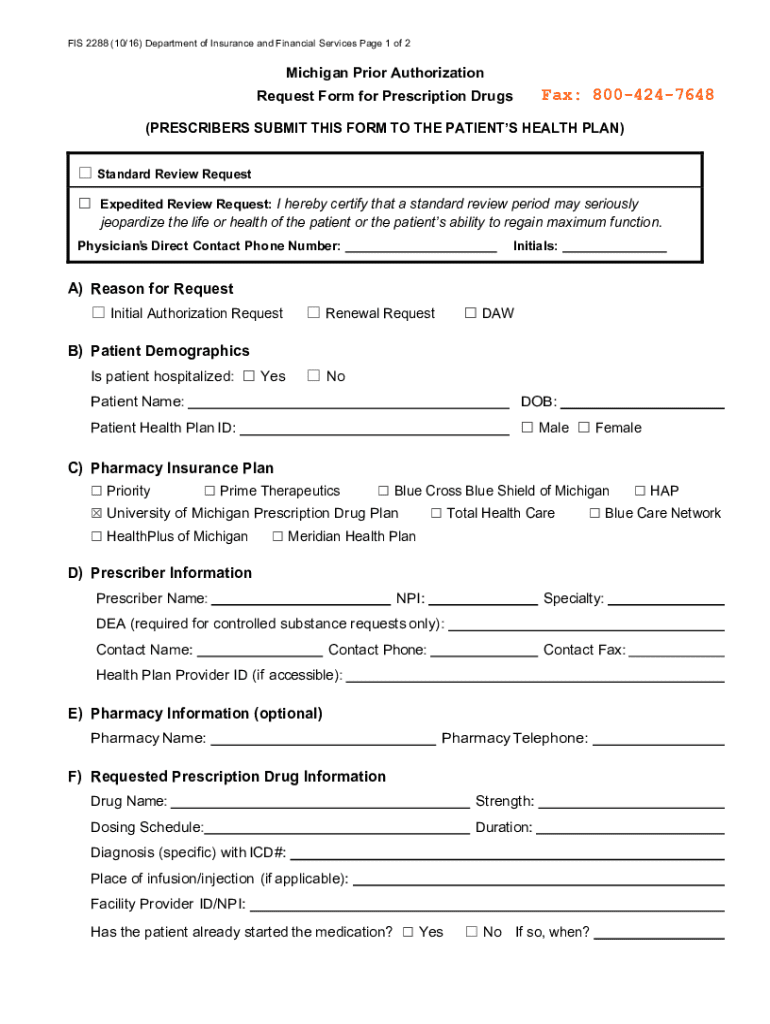
A Comprehensive Guide to the Michigan Prior Authorization Request Form
Understanding prior authorization in Michigan
Prior authorization is a critical mechanism in Michigan's healthcare system, designed to control costs and ensure that patients receive appropriate treatments. It is a requirement imposed by insurers where healthcare providers must seek approval before a specific service or treatment is delivered. This process is essential for managing patient care effectively, ensuring that the treatments proposed align with best practices and are medically necessary.
The prior authorization process in Michigan typically involves submitting a request along with relevant clinical information to the patient's insurance provider. The insurer then reviews the details and determines whether to grant the authorization based on their policies and guidelines, ultimately influencing the patient's ability to access prescribed services.
Key components of the Michigan prior authorization request form
Completing the Michigan prior authorization request form requires precise information to ensure a smooth approval process. The essential details include the patient's demographic data, provider information, and specifics of the services or treatments requested. All information must be accurate and up-to-date.
In addition to the request form, supporting documentation is often necessary to substantiate the medical need for the requested treatment. This can include clinical notes, lab results, and any previous treatment history.
Supporting documentation
Necessary medical documentation varies depending on the specific treatment or service being requested. To streamline the process, submitting common templates can significantly reduce review times. These templates may include prior treatment summaries, referral letters, or specific tests required to support the necessity of the service.
Step-by-step guide to completing the Michigan prior authorization request form
Completing the Michigan prior authorization request form can be streamlined by following these steps. First, begin by gathering all necessary information and documentation to populate the form thoroughly.
Accurate completion of the form is crucial, as errors can lead to delays in the approval process.
Common challenges and solutions when using the prior authorization request form
While utilizing the Michigan prior authorization request form can be straightforward, several common challenges may arise. Incomplete forms and missing supporting documentation can significantly hinder the authorization process.
To troubleshoot submission issues, consider maintaining a checklist of all required elements to ensure no details are overlooked.
Interactive tools for managing your prior authorization requests
With the rise of digital solutions, various online tools have emerged to help healthcare providers manage prior authorization requests effectively. These platforms can greatly enhance the process.
By choosing a comprehensive tool like pdfFiller, healthcare professionals can save time and enhance the likelihood of successful authorization.
Tracking and following up on your prior authorization request
After submitting the Michigan prior authorization request form, it's pivotal to track the status of your submission actively. This can help address any outstanding requirements before they delay patient care.
Being proactive in this phase can greatly improve the efficiency of the authorization process.
Special considerations for specific treatments or medications
Certain treatments or medications might have unique requirements when it comes to prior authorization in Michigan. For example, high-cost medications often require extensive documentation to justify their necessity.
Understanding the specific protocols for these unique cases can aid in a smoother authorization process.
Tips for successful prior authorization approval
To increase the likelihood of obtaining prior authorization, it's essential to follow strategic practices. Thorough understanding of insurance plans and effective communication can prove beneficial.
Implementing these strategies can significantly boost the success rate of authorization applications.
Accessing resources and support for prior authorization
For those navigating the complexities of the Michigan prior authorization process, several resources are available. Contacting state-insurers or seeking guidance from professional associations is invaluable for staying informed.
Staying connected with these resources can empower individuals and teams when navigating complex prior authorization processes.
FAQs about the Michigan prior authorization request process
Understanding the frequently asked questions regarding the Michigan prior authorization process can alleviate many concerns surrounding it. Engaging with these questions provides clarity on what's expected...
Educating oneself on these aspects can streamline the experience significantly.
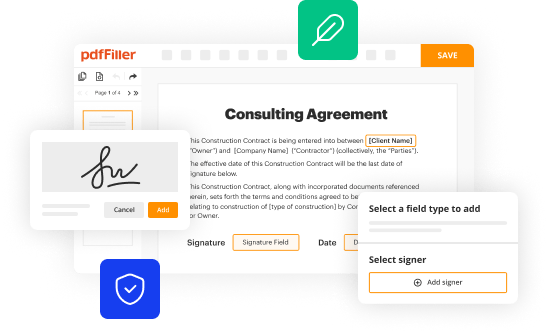
How pdfFiller enhances the prior authorization experience
PdfFiller stands out in the document management landscape, particularly in streamlining the prior authorization process. Its comprehensive features allow users to navigate complex forms like the Michigan prior authorization request form more efficiently.
Adopting pdfFiller not only simplifies the prior authorization request process but also enhances overall healthcare efficiency in a digital-first world.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I modify my michigan prior authorization request in Gmail?
How do I edit michigan prior authorization request online?
Can I create an electronic signature for signing my michigan prior authorization request in Gmail?
What is michigan prior authorization request?
Who is required to file michigan prior authorization request?
How to fill out michigan prior authorization request?
What is the purpose of michigan prior authorization request?
What information must be reported on michigan prior authorization request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.