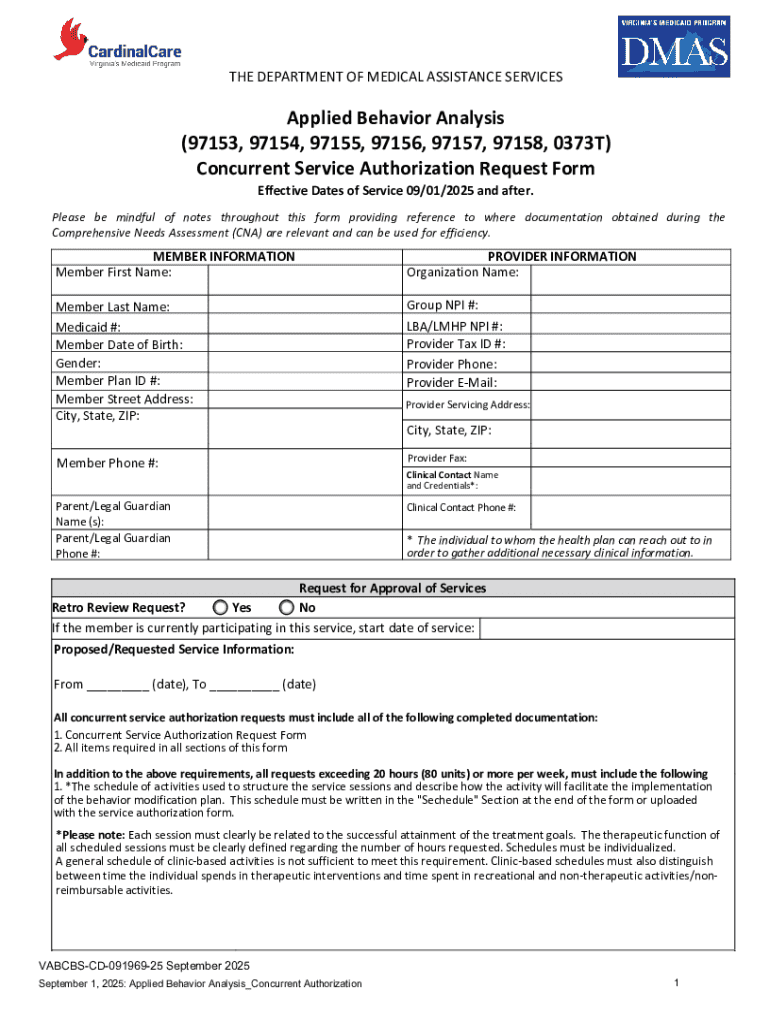
Get the free Concurrent Service Authorization Request Form
Get, Create, Make and Sign concurrent service authorization request
Editing concurrent service authorization request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out concurrent service authorization request
How to fill out concurrent service authorization request
Who needs concurrent service authorization request?
A comprehensive guide to the concurrent service authorization request form
Understanding the concurrent service authorization request
A concurrent service authorization request is essential in navigating the intersection of healthcare services and insurance processes. It allows healthcare providers to seek permission from insurers to proceed with specific services that may not automatically be covered under a patient's plan. This process ensures that patients receive necessary care while adhering to their insurance coverage guidelines.
The importance of this authorization cannot be understated. It safeguards the interests of patients by confirming that the services they receive align with their insurance policies, thereby minimizing unexpected out-of-pocket expenses. It also assists healthcare providers in delivering care that is both efficient and financially viable.
Importance of accurate documentation
Accurate documentation is crucial in the process of submitting a concurrent service authorization request form. Inaccurate or incomplete forms can lead to significant delays in treatment approval, which can be detrimental to a patient's health. For healthcare providers, these mistakes can translate to wasted resources and increased administrative burdens.
Moreover, cultural relevance plays a significant role in healthcare eligibility and insurance processes. For diverse populations, ensuring that authorization forms are culturally sensitive and accessible can greatly affect the overall experience of securing care.
Overview of the concurrent service authorization process
The concurrent service authorization process involves several key stakeholders, each playing a vital role in ensuring the smooth operation of service provision. Healthcare providers initiate the requests on behalf of their patients, submitting pertinent information necessary for insurers to understand and approve the request.
Patients and their caregivers also play an integral part; they must be informed and sometimes assist in gathering necessary documentation. Insurers have their own set of requirements that must be met for the authorization to be granted, creating a collaborative yet complex web of accountability.
Typically, several types of services require concurrent authorization, including medical services like surgeries and diagnostics, behavioral health services, and pharmacy services where medications are involved. Each of these categories might have unique requirements based on the insurance policy parameters.
Step-by-step guide to completing the concurrent service authorization request form
Completing the concurrent service authorization request form effectively starts with gathering necessary information. This includes essential patient details such as their full name, date of birth, and insurance information. Additionally, providers must include their details — including credentials and contact information — and a thorough description of the requested service.
Whether submitting forms online, via fax, or by mail, ensuring timely processing often relies on the completeness and accuracy of the submitted information. Each section of the form should be filled meticulously, paying special attention to any specific instructions provided on the form itself.
Common mistakes to avoid typically arise from omitting key patient information or failing to provide sufficient detail concerning the medical necessity of the requested services. Double-checking each section against the original requirements set forth by the insurer can help mitigate these risks.
Tips for successful authorization requests
For healthcare providers, following best practices during the submission process can enhance the chances of authorization approval. Communication with insurance companies before submission can clarify any ambiguities and ensure the request meets all preliminary requirements. Providers should emphasize the clinical necessity in their documentation by including supportive evidence or patient history that justifies the need for the service.
In instances where authorization is denied, knowing how to navigate denials and appeals effectively is crucial. Providers should familiarize themselves with common reasons for denials, such as lack of medical necessity or incomplete information, and prepare to present compelling evidence when appealing these decisions.
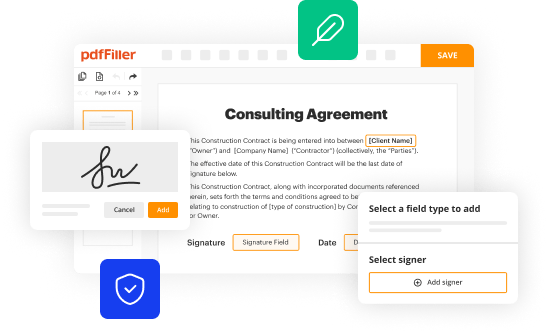
Managing authorization requests with pdfFiller
pdfFiller greatly simplifies the process of completing the concurrent service authorization request form. By offering tools that streamline document editing and signing, pdfFiller enables healthcare teams to manage their requests efficiently from any location. This eliminates the complications that often arise from paper-based submission processes.
Collaborative tools within pdfFiller allow teams to work together seamlessly, ensuring that every piece of documentation is accurate and up-to-date. With features that support easy access and secure storage, providers can stay organized while managing multiple requests.
Frequently asked questions (FAQs)
When submitting a concurrent service authorization request form, many users frequently encounter common queries. For instance, what should you do if your request is denied? It's important to review the denial letter carefully, understand the reason, and seek guidance on how to appeal the decision effectively.
Another common question often revolves around the timeline for processing authorizations. Typically, insurers are required to respond to requests within a specific period, but this can vary significantly depending on the insurer and the type of service requested. Additionally, some providers may find themselves looking for ways to expedite their requests if there are urgent health concerns at play.
Contacting support for assistance
If you find yourself struggling with the concurrent service authorization request form, pdfFiller offers comprehensive customer support options. Users can reach out via live chat, email, or phone to get the help they need. This level of accessibility ensures that questions can be addressed promptly, allowing users to navigate the documentation process effectively.
Additionally, pdfFiller has prepared various resources specifically geared towards both providers and patients, including detailed manuals and instructional guides that assist users in understanding the complexities of authorization requests. Having access to these materials ensures you are well-equipped to handle any challenges that arise.
Utilizing pdfFiller’s interactive tools
pdfFiller is equipped with various interactive tools designed to optimize how users complete and manage their concurrent service authorization request forms. With customizable templates that cater to different types of authorization requests, healthcare providers can save valuable time and ensure access to the latest forms.
Furthermore, pdfFiller’s collaborative spaces facilitate team reviews, allowing multiple stakeholders to engage in the editing process. This enhances compliance and accuracy, especially in the context of evolving healthcare regulations and authorization requirements. The platform’s adaptability means that it can be tailored to suit specific operational needs for healthcare providers.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I manage my concurrent service authorization request directly from Gmail?
How do I edit concurrent service authorization request on an iOS device?
How do I complete concurrent service authorization request on an Android device?
What is concurrent service authorization request?
Who is required to file concurrent service authorization request?
How to fill out concurrent service authorization request?
What is the purpose of concurrent service authorization request?
What information must be reported on concurrent service authorization request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.