Get the free COVID-19 exposed systemic weak points. How to get it ...
Get, Create, Make and Sign covid-19 exposed systemic weak
Editing covid-19 exposed systemic weak online
Uncompromising security for your PDF editing and eSignature needs
How to fill out covid-19 exposed systemic weak
How to fill out covid-19 exposed systemic weak
Who needs covid-19 exposed systemic weak?
COVID-19 Exposed Systemic Weak Form
Understanding systemic weaknesses in health systems
Systemic weaknesses in health systems refer to the vulnerabilities and gaps that exist within healthcare infrastructures, which limit their ability to effectively respond to public health crises. COVID-19 has starkly exposed these frailties, revealing how unprepared many systems were for a pandemic of such magnitude. The virus did not discriminate; it laid bare the deficiencies in how health systems are organized, funded, and managed.
Key areas of concern that emerged can be outlined as follows:
Key findings from COVID-19 impact assessment
Data-driven insights reveal the stark reality of systemic failures. Various assessments, including evaluations by the American Medical Association and health policy experts, highlighted critical moments where the healthcare system faltered. For example, during the initial wave of infections, hospitals were overwhelmed with patients, leading to resource shortages and increased mortality rates.
Case studies from different countries illustrated these findings. In Italy, the healthcare system faced collapse early in the pandemic, revealing urgent needs for better resource allocation and management. Lessons learned reveal the importance of rapid response mechanisms and the necessity for clear communication among all stakeholders involved in healthcare delivery.
Recommendations for strengthening health systems
As we move forward, several comprehensive strategies can fortify health systems against future crises. First, investing in public health preparedness is paramount. Enhanced funding and resources should target vital areas such as surveillance, laboratory capabilities, and community health initiatives.
Second, as telehealth has gained importance, enhancing remote services can ensure consistent patient care, minimizing exposure during outbreaks. Third, ensuring equitable access to care remains critical. Policymakers must focus on eliminating barriers that prevent disadvantaged populations from receiving necessary healthcare. Alongside these measures, community engagement and education initiatives will empower individuals to take proactive roles in their health.
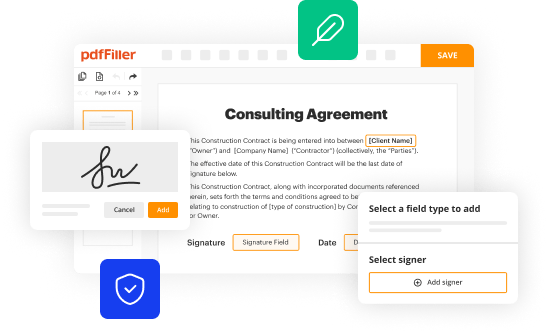
Role of digital tools in addressing weak points
Digital tools have become invaluable in reforming healthcare processes. Platforms like pdfFiller facilitate operational efficiency through streamlined document management, which can improve many health services. Effective document handling ensures timely patient care and efficient communication among healthcare teams.
Utilizing digital tools allows for e-signatures and document edits that support telehealth initiatives. Ensuring privacy and compliance in documentation remains paramount, and the integration of interactive tools serves to track and manage health data more effectively.
Best practices for document management in healthcare
Creating patient-centered documents is essential in improving health outcomes. Healthcare providers should focus on clarity and accessibility for patients, ensuring that forms are easy to understand and fill out. Utilizing templates effectively helps streamline this process.
In addition, customizable forms for various healthcare needs can promote a standardized approach to documentation, minimizing errors. Collaborating with teams using cloud-based tools enhances productivity and ensures all members stay updated on patient care requirements.
Training and empowering healthcare providers
Developing training programs for healthcare personnel is vital for equipping them with the knowledge required to navigate future systemic challenges. Training should emphasize adaptability and continuous education to keep pace with evolving public health demands. Engaging future physicians in addressing systemic issues, such as promoting practices that enhance health equity and access, is essential.
A well-equipped workforce that understands the intricacies of health policy, including the significance of food labels and health benefits such as low-sugar and low-salt diets, can drive meaningful change within communities. Empowering healthcare professionals reduces gaps and improves responses during emergencies.
Collaborative approaches to reforming healthcare
Collaborative efforts among stakeholders significantly enhance the reform process. Building partnerships between government entities, healthcare providers, and technology firms fosters innovative solutions that address systemic weaknesses. Successful case studies demonstrate how collective action can streamline services.
Innovative models for integrated care, highlighting the importance of collaborative frameworks, show that such partnerships result in better health outcomes and reduced care fragmentation. These collaborative efforts should focus on sustainable approaches that not only address immediate needs but also pave the way for future resilience.
Conclusion: A vision for a resilient future
To forge a roadmap for implementing recommended changes, it is crucial to encourage proactive planning that goes beyond mere crisis management. Continuous evaluation and adaptation of health policies will create a dynamic system that can respond efficiently to the evolving landscape of public health.
Establishing a resilient healthcare system requires commitment from all sectors—policy frameworks, technological investment, and community involvement. Only through a multi-faceted approach can we ensure our health systems are equipped to handle the next public health threat effectively.
Interactive elements for deeper engagement
Incorporating interactive tools within platforms like pdfFiller can facilitate easier document creation and management. These resources allow users to explore systemic health reforms while providing valuable insights on best practices.
Embedding helpful tools can also guide healthcare teams in efficiently managing and signing documents, contributing to a streamlined operational process. By prioritizing usability and engagement, pdfFiller empowers users to navigate health-related documentation seamlessly.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I execute covid-19 exposed systemic weak online?
How do I fill out the covid-19 exposed systemic weak form on my smartphone?
How do I complete covid-19 exposed systemic weak on an iOS device?
What is covid-19 exposed systemic weak?
Who is required to file covid-19 exposed systemic weak?
How to fill out covid-19 exposed systemic weak?
What is the purpose of covid-19 exposed systemic weak?
What information must be reported on covid-19 exposed systemic weak?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.