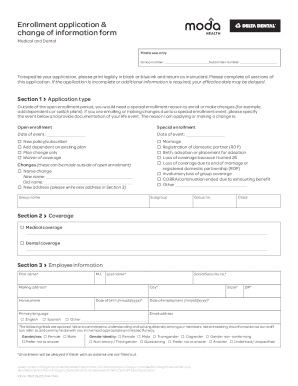
Get the free Molina Healthcare Service Authorization (sa) Form
Get, Create, Make and Sign molina healthcare service authorization



Editing molina healthcare service authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out molina healthcare service authorization

How to fill out molina healthcare service authorization
Who needs molina healthcare service authorization?
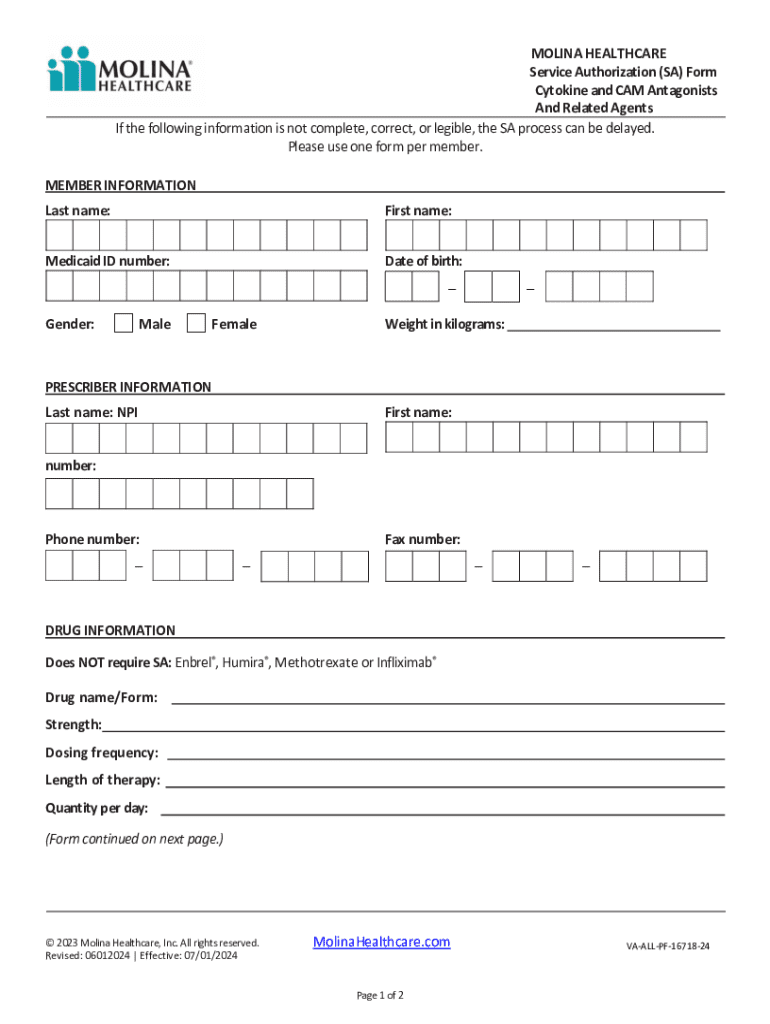
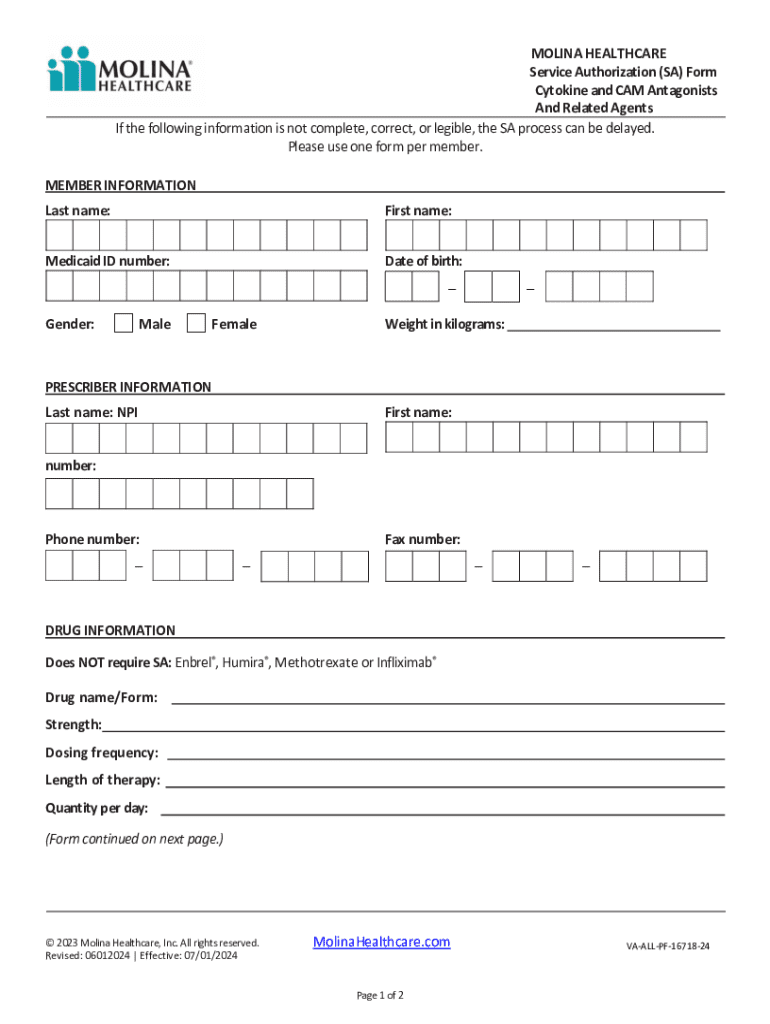
Understanding the Molina Healthcare Service Authorization Form
Overview of Molina Healthcare Service Authorization Form
The Molina Healthcare Service Authorization Form is a critical document used within the Molina Healthcare system that enables patients to access medically necessary services. This form is designed to obtain prior authorization before certain types of healthcare services are rendered, ensuring that patients receive appropriate and covered services under their health plans.
The significance of the service authorization cannot be overstated. It serves as a safeguard for both healthcare providers and patients, ensuring that requested services are medically justified and covered by the patient's health insurance policy. By streamlining the authorization process, Molina Healthcare ensures that patients can receive timely access to the treatments they need.
Key features of the Molina Healthcare Authorization Form include clarity in documenting patient information, detailed service request information, and a structured approval process that prioritizes urgency and medical necessity.
Who needs the Molina Healthcare Service Authorization Form?
The Molina Healthcare Service Authorization Form is primarily intended for patients who require specific healthcare services that mandate prior approval. This form can be necessary for a wide range of individuals seeking treatments such as surgeries, diagnostic imaging, specialized therapy, and other potentially costly or uncommon medical services.
Eligibility for services requiring this form typically encompasses individuals who are enrolled in a Molina Healthcare plan. Specific criteria for authorization generally depend on factors including the type of service requested, the patient’s health condition, and the necessity of the treatment based on clinical guidelines.
Understanding the authorization process
Navigating the Molina Healthcare authorization process involves several key steps that ensure all relevant information is captured accurately. First, it is essential to gather all necessary information, including the patient's medical history, current medications, and other relevant clinical details. This information provides healthcare providers the groundwork for justifying the need for the requested service.
The next step is completing the authorization form itself, which requires detailed input about the patient, the service provider, and the specific nature of the service requested. Once the form is fully completed, it needs to be submitted promptly, either electronically or via traditional means, depending on the preferences of the involved parties.
It's important to familiarize oneself with the expected timeframe for approval after submission. Generally, authorization requests can take anywhere from a few days to several weeks depending on the complexity of the service requested and the volume of requests being processed.
Detailed instructions for filling out the Molina Healthcare Service Authorization Form
Filling out the Molina Healthcare Service Authorization Form accurately is crucial. Each section of the form is designed to capture essential information needed for effective processing and approval.
Key sections of the form include:
Common mistakes to avoid include incomplete entries, missing signatures, and incorrect patient information, which could lead to delays or denials in authorization.
Editing and managing your authorization form with pdfFiller
Leveraging tools like pdfFiller can significantly ease the process of managing the Molina Healthcare Service Authorization Form. It provides users with robust editing capabilities that allow for quick adjustments to the form as needed, ensuring accuracy and completeness.
Additionally, pdfFiller offers eSignature options that enable both patients and providers to sign the authorization form securely. This functionality facilitates a streamlined approval process by ensuring all necessary parties endorse the document without the hassles of physical signatures.
Real-time collaboration features are another highlight, letting care teams work together to complete and manage authorization requests efficiently. This collaborative approach reduces the risk of errors and improves communication among healthcare professionals.
Frequently asked questions (FAQs) about the Molina Healthcare Service Authorization Form
The authorization process often brings up various questions. Here are some frequently asked queries about the Molina Healthcare Service Authorization Form.
Interactive tools and resources available on pdfFiller
pdfFiller provides a wealth of interactive tools and resources designed to enhance user experience when managing authorization forms. One key feature is access to a vast library of form templates, which allows users to find the appropriate authorization forms they need with ease.
Additionally, comprehensive tutorials guide users through each step of form management. These resources are particularly beneficial for those new to managing service authorizations, providing clarity and guidance throughout the process.
The real-time collaboration capabilities enable users to share documents with healthcare professionals for input, making the authorization process smooth and efficient.
Final tips for efficiently managing your Molina Healthcare Service Authorization Form
Efficiently managing the Molina Healthcare Service Authorization Form requires diligence and organization. Keeping track of your authorization status is crucial; be proactive and follow up periodically with Molina’s customer service if updates are not communicated promptly.
Implementing best practices for document management will enhance the likelihood of successful authorizations. Store all relevant documents electronically for easy access and ensure documents are updated regularly, particularly if there are changes in the patient's health or treatment plan.
Utilizing cloud-based solutions such as pdfFiller allows for seamless access and management of forms, ensuring that you can easily make necessary updates and collaborate with relevant parties from any location.
Contact information for assistance
For individuals needing further assistance with the Molina Healthcare Service Authorization Form, contacting Molina Healthcare's customer service is recommended. They can provide clarity on specific policies and help navigate any issues.
To access support through pdfFiller, users can take advantage of online help resources, including tutorials, FAQs, and community forums designed for collaboration and assistance.
Additionally, engaging in community help forums can provide insight from peers who may have encountered similar issues, enriching your understanding of the authorization process.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I send molina healthcare service authorization to be eSigned by others?
How do I make changes in molina healthcare service authorization?
How do I edit molina healthcare service authorization on an iOS device?
What is molina healthcare service authorization?
Who is required to file molina healthcare service authorization?
How to fill out molina healthcare service authorization?
What is the purpose of molina healthcare service authorization?
What information must be reported on molina healthcare service authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.