Understanding the Patient Authorization to Release Form
Understanding the Patient Authorization to Release Form
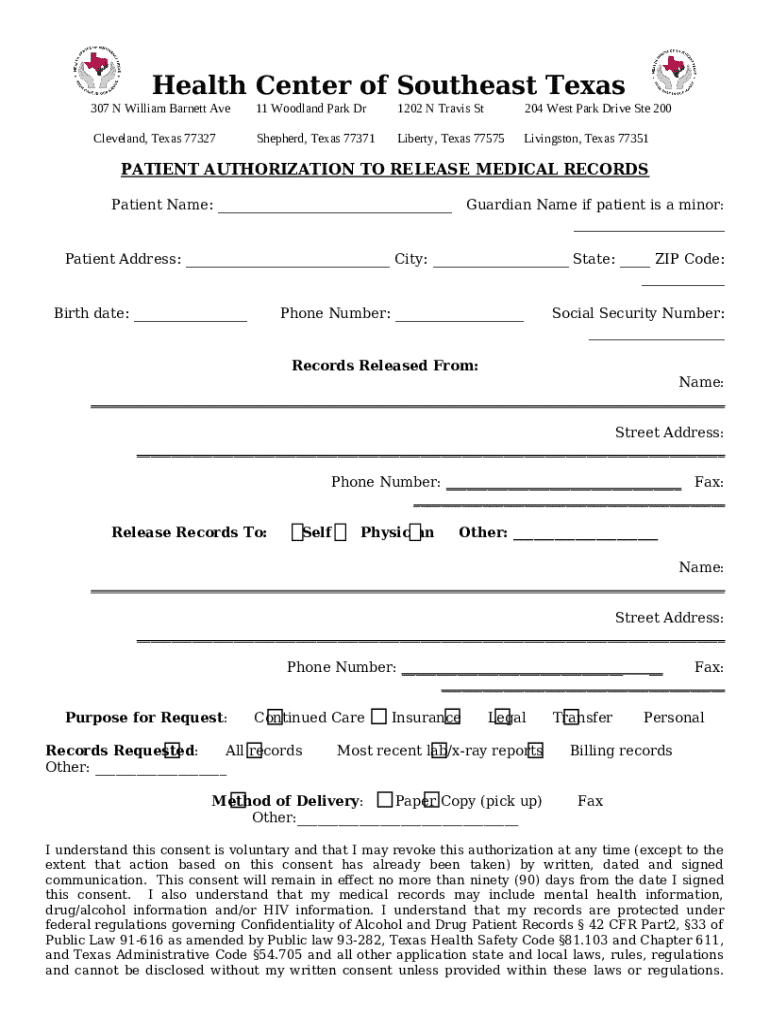
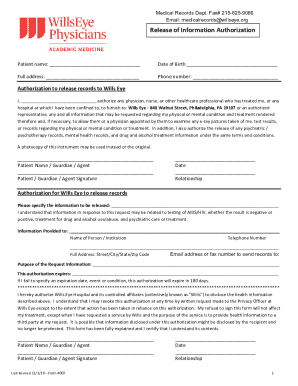
The patient authorization to release form is a crucial document in the healthcare process, ensuring that patient privacy is maintained while facilitating communication between healthcare providers. This form grants permission for a third party, often a healthcare provider or family member, to access a patient’s medical records or specific health information. It plays a vital role in preserving patient confidentiality and trust, particularly as healthcare systems become increasingly interconnected.
In the realm of healthcare, maintaining the confidentiality of patient information is paramount. The patient authorization to release form acts as a protective barrier ensuring that patient data is only shared when explicitly permitted. This not only reinforces ethical practices within healthcare but also adheres to regulatory standards set by laws such as the Health Insurance Portability and Accountability Act (HIPAA).
Key components of the form
Includes full name, date of birth, and contact information.
Details of the individual or organization receiving the information.
Specification of what medical records or data are being shared.
Patient's signature to confirm authorization and the date of signing.
When is a patient authorization to release form needed?
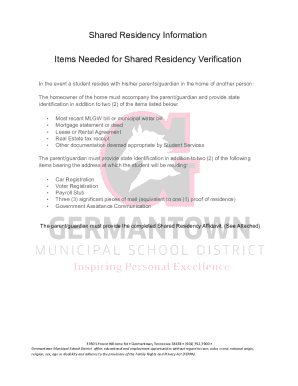
Authorization forms are essential in various situations in which patient data must be shared. Often, healthcare providers require such forms before accessing or disclosing a patient’s medical records. This is particularly important when transitioning care between providers, substantiating insurance claims, or involving legal requirements. By requiring explicit consent through a patient authorization to release form, healthcare organizations adhere to legal standards while respecting patient autonomy.
There are several common scenarios wherein this form is utilized, such as:
When patients switch doctors, the new provider may need access to past medical records to ensure continuity of care.
Insurance companies often require specific patient information to process claims accurately.
Participants may need their medical information shared for research purposes, necessitating their consent.
How to fill out the patient authorization to release form
Filling out the patient authorization to release form requires careful attention to detail to ensure compliance and effectiveness. Following a structured approach will help minimize errors and misunderstanding.
Here’s a step-by-step guide:
Compile personal identification details of both the patient and the person or organization to whom the information will be released.
Double-check accuracy of the patient’s name, contact information, and birth date to prevent any mix-ups.
Clearly specify who will receive the information, ensuring their correct identification.
Be specific about the type of medical records being released; avoid vague language.
Indicate how long the authorization remains valid, which can range from specific dates to indefinitely until revoked.
Ensure that the patient (and, where required, a witness) signs the form. This step often is a legal requirement.
Common mistakes to avoid include omitting critical information and misunderstanding expiration dates. A small error can delay necessary healthcare processes.
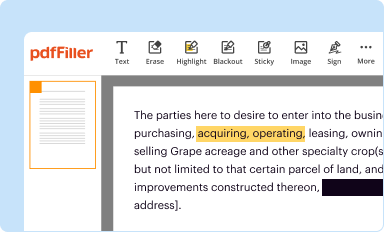
Editing and customizing the form
Customizing the patient authorization to release form can enhance its clarity and usability. Tools like pdfFiller allow users to edit documents efficiently without needing extensive technical knowledge.
To customize using pdfFiller, follow these steps:
Easily import the form into the platform for editing.
Make changes directly on the document, using features that allow text modification, highlighting, or annotation.
Incorporate fields for future entries, ensuring the document meets personalized needs.
The benefit of customizing the form lies in tailoring it to specific needs, ensuring clarity regarding the information being shared while remaining compliant with healthcare regulations.
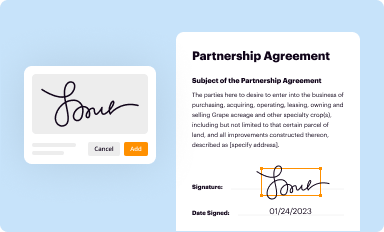
Digitally signing the patient authorization to release form
Digital signatures are increasingly gaining acceptance in the healthcare domain, offering a practical solution to the traditional pen-and-paper signing processes. Embracing eSigning enhances efficiency while maintaining legal robustness.
Steps to eSign using pdfFiller include:
Follow the platform's guided process to design a unique signature.
Easily place the signature on the designated line through intuitive drag-and-drop functionality.
Once signed, verifying signatures for authenticity is crucial to uphold security and compliance. Ensure the signing process complies with legal standards pertinent to your locality.
Managing the completed form
The management of the completed patient authorization to release form is just as vital as completing it. Securing the information contained within this document contributes to ongoing patient privacy.
Here are ways to effectively manage the completed form:
Leverage cloud storage features to ensure documents are safeguarded against unauthorized access.
Facilitate secure sharing utilizing unique links or direct uploads to relevant healthcare systems.
Moreover, tracking the release of information is crucial. Knowing who has access to the form protects the patient's privacy while also helping to uphold regulatory compliance.
Legal considerations and patient rights
Navigating the legal landscape surrounding medical records and patient privacy is essential. The HIPAA regulations outline fundamental rights that govern patient information sharing, stipulating that all releases must be authorized.
Patients have the right to revoke their consent at any time, provided that they follow proper procedures. In a scenario where unauthorized disclosures occur, patients must understand their recourse, which may include reporting to regulatory bodies and pursuing legal action if necessary.
Frequently asked questions (FAQs)
Patients often have questions regarding the patient authorization to release form. Common queries include concerns about what happens if information needs to be changed after submission. Generally, patients can issue a new authorization or amend existing permissions without difficulty.
Another frequent question is whether someone else can fill out the form on behalf of the patient. With proper documentation or legal authority, this is acceptable in many situations. Additionally, patients should be aware that while verbal authorization or informal agreements may suffice in certain cases, such practices are not standard for all healthcare settings.
Final thoughts on the patient authorization to release form
A thorough understanding of the patient authorization to release form helps patients navigate their interactions with the healthcare system more effectively. It promotes independence and control over personal medical information, fostering an environment of trust between patients and providers.
Best practices for patients and healthcare teams involve open communication about patient information needs. This collaboration not only ensures compliance but strengthens the patient care experience, resulting in improved outcomes for all parties.