A comprehensive guide to requesting restrictions on PHI forms
Understanding the PHI (Protected Health Information) concept
Protected Health Information (PHI) refers to any health information that can identify an individual and is stored, transmitted, or received by a healthcare provider, health plan, or healthcare clearinghouse. The importance of PHI in healthcare cannot be overstated, as it encompasses sensitive data that, if disclosed, can lead to privacy breaches and identity theft. The safeguarding of PHI is primarily governed by the Health Insurance Portability and Accountability Act of 1996 (HIPAA), which sets standards for protecting individuals' medical records and other personal health information.
Common scenarios involving PHI include patient records, billing information, medical histories, and treatment plans. Each instance requires strict adherence to confidentiality and consent regulations, ensuring that only authorized personnel have access to this sensitive information.
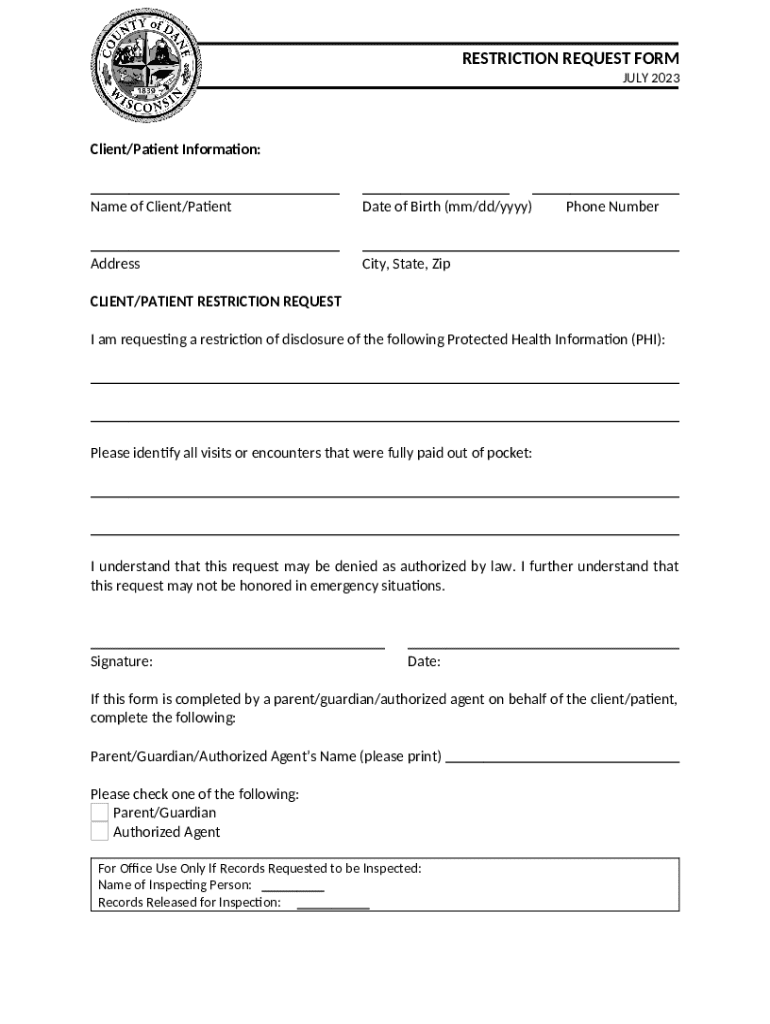
What is a Request Restriction on PHI form?
The Request Restriction on PHI Form is a pivotal document that allows patients to request limitations on the disclosure of their health information. This request is crucial for individuals concerned about certain aspects of their health data being shared with third parties, including insurers or external healthcare providers. Filling out this form is an expression of a patient's rights and desires regarding their health information privacy.
Patients, caregivers, or legal representatives can fill out this form. The significance lies in its ability to provide patients with autonomy over their health information, establishing boundaries around who can access which specific data. Key legal and ethical considerations center around the patient's rights under HIPAA, emphasizing the importance of informed consent and personal control over health-related data.
When to use the Request Restriction on PHI form
Certain circumstances may prompt a patient to submit a Request Restriction on PHI Form. Common instances include feelings of uncertainty about the sharing of health information with insurers, fears of stigma associated with specific health conditions, and concerns about family members accessing particular health details. In situations where a patient knows that certain data could be misused or lead to undesired consequences, a restriction can provide peace of mind.
Examples of common requests include limiting disclosures to specific healthcare providers or insurers, or entirely restricting access to certain mental health records. Understanding these implications is crucial as they may affect the continuity of care or affect coverage and treatment decisions.
Detailed instructions for filling out the form
Filling out the Request Restriction on PHI Form can seem overwhelming without guidance. The form typically includes several critical sections. The personal information section requires the patient's name, date of birth, and contact details, essential for the healthcare provider to identify the individual clearly.
Next, the applicant specifies the restrictions requested. This is the most important part of the form, where clarity is vital. Patients should articulate precisely which disclosures they wish to limit and to whom they wish these limitations to apply. For example, stating that they do not want their information shared with a particular insurance company or healthcare provider is essential. Common mistakes to avoid include submitting incomplete forms, failing to be specific about restrictions, or not providing valid contact information for follow-up communications.
Submitting your request
After filling out the Request Restriction on PHI Form, understanding the submission process is vital. Various acceptable methods include online submissions through platforms like pdfFiller, mailing the paper form directly to the healthcare provider, or faxing the request. Online submissions offer the advantage of being easily trackable and generally faster.
Once the request is submitted, patients should keep a copy and note the date of submission. Tracking the request status may involve following up with the provider’s office. Patients should also understand typical response times, which often range from a few days to several weeks, depending on the facility.
What happens after submission?
The process following the submission of the Request Restriction on PHI Form involves a review by the healthcare organization. This review can result in various outcomes: approval, denial, or a request for clarification from the provider. It’s crucial to know patients' rights if a request is denied; understanding the rationale behind the denial is essential, and patients have the right to ask for a detailed explanation.
If denied, patients can explore how to appeal the decision effectively. This often involves providing additional information or clarification to support the reason for the request.
Managing and modifying your restrictions
As circumstances change, patients may need to update or revoke restrictions on their PHI. This process is generally straightforward but requires filling out a new request form indicating the desired changes. Important considerations include ensuring that new restrictions do not negatively impact necessary disclosures for treatment purposes.
Using platforms like pdfFiller, patients can streamline this process by keeping their documents organized and easily updatable, allowing for efficient document management.
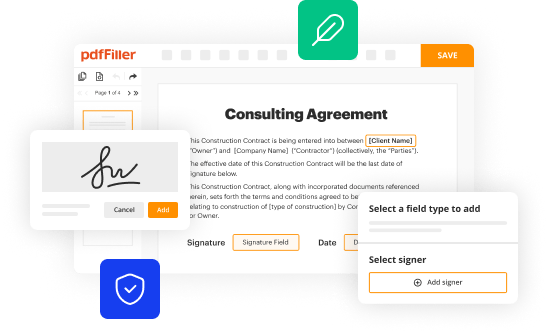
Interactive tools and resources available on pdfFiller
pdfFiller offers a range of interactive tools to assist users in managing their Request Restriction on PHI Forms effectively. The platform allows users to edit and customize forms easily, adapting them to their specific circumstances. Step-by-step video tutorials simplify the process of completing the PHI restriction request, providing valuable visual guidance.
Additionally, collaboration tools are available for teams, making it easier to share documents and streamline the management process, ensuring that everyone involved can stay informed and organized.
Case studies and real-life examples
In exploring case studies of successful restriction requests, one can find numerous instances where patients effectively limited access to their sensitive health information. These successful requests often stem from clear communication and well-articulated concerns. For instance, a patient concerned about the disclosure of their mental health history to an employer requested restrictions, which were granted after the provider understood the patient's context.
Conversely, there are lessons to be learned from denied requests. An example includes a patient whose request was denied because the restrictions hindered necessary communication regarding treatment continuity. This highlights the need for patients to balance their privacy desires with the need for effective healthcare delivery.
Frequently asked questions (FAQs)
Generally, common queries about the Request Restriction on PHI Form arise frequently. One common concern is, 'What if my healthcare provider denies my request?' In such cases, patients can inquire about the specific reasons for the denial to better understand the situation and potentially address any gaps in their request.
'Can I request a restriction on all my health information?' is another frequent question. While patients have the right to request restrictions, healthcare providers are not obligated to accept blanket restrictions and can negotiate specific limits based on operational and clinical necessities.
Best practices for safeguarding your health information
After submitting a request for restriction, continuous safeguarding of one's health information remains vital. Patients should utilize pdfFiller's features to keep documents organized and secure, maintaining proactive control over their personal data. This includes maintaining clear communication lines with healthcare providers regarding the status of their requests and any changes in their health information needs.
Encouraging proactive communication not only helps safeguard information but also ensures that care providers remain informed about patients' privacy preferences and needs, enhancing the overall healthcare experience.