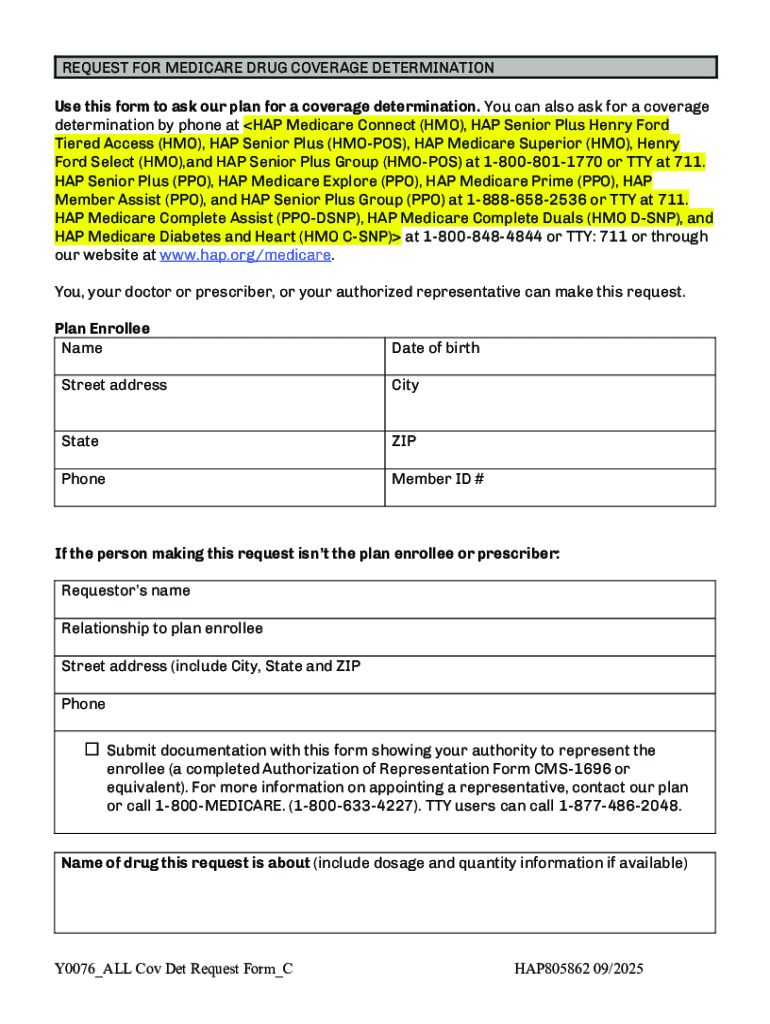
Get the free Coverage Determination Request Form 2026. Prescription drug coverage determination
Get, Create, Make and Sign coverage determination request form
Editing coverage determination request form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out coverage determination request form
How to fill out coverage determination request form
Who needs coverage determination request form?
Coverage Determination Request Form: A Comprehensive How-to Guide
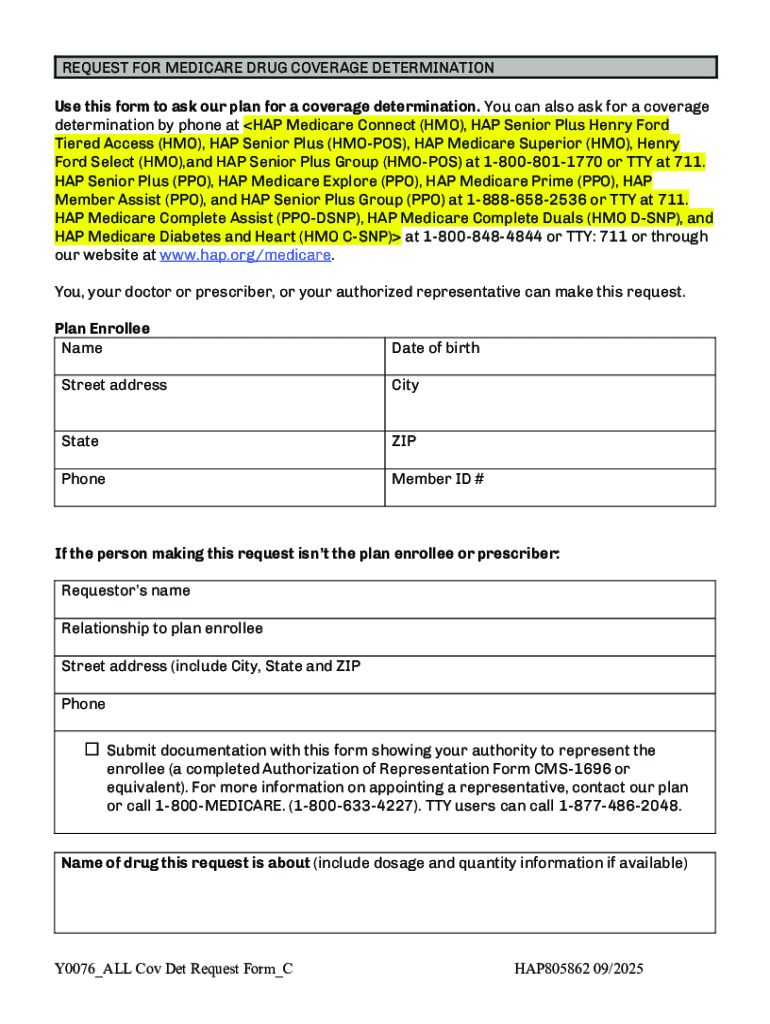
Overview of coverage determination request forms
A coverage determination request form is a crucial document in the healthcare and insurance landscape, enabling patients and healthcare providers to seek clarity on whether a specific service, treatment, or medication is covered by an insurance plan. The purpose of this form is to formally request a decision from the insurance provider regarding coverage for treatments that may not be routinely covered or require additional justification, such as specialized services or higher-cost medications.
These forms not only streamline the communication process between providers and insurance companies but also ensure that patients receive the necessary care with minimal financial barriers. Completing a coverage determination request form accurately is integral for navigating complex insurance systems and receiving timely approval for necessary treatments.
Understanding coverage determination
Coverage determination refers to the assessment made by insurance providers to establish whether a claim will be accepted based on the policyholder's coverage. Patients, especially those with chronic conditions or specialized treatment needs, often require a coverage determination to ascertain the approval of necessary services, like surgeries or expensive medications. Essentially, it answers the critical question: 'Is this treatment covered under my plan?'
Anyone utilizing health insurance may need a coverage determination at some point. This can include patients facing rare medical conditions or those requiring advanced treatments not broadly covered by their policies. Submitting this request is especially pertinent when patients wish to access specific medications or services not typically included in their plan’s standard coverage list.
The timing for when to submit a coverage determination request is essential; doing so proactively can prevent delays in treatment. Ideally, requests should be filled out and submitted as soon as a provider recommends a treatment requiring approval to minimize disruptions in care.
Steps to complete a coverage determination request form
Completing a coverage determination request form involves several methodical steps to ensure that you have all the necessary information readily accessible, and that your request is submitted correctly.
Navigating common challenges
While completing a coverage determination request form is straightforward, challenges can arise that may complicate the process. One common issue is delays in processing times, particularly if forms are submitted without complete information. These delays can be incredibly frustrating for patients eager to start their treatment.
Another frequent challenge comes in the form of denial reasons. Denials can occur for various reasons, such as not meeting the insurer’s criteria or submitting documentation that lacks sufficient detail. Addressing these denials may involve providing additional information or clarifications and leveraging the support of healthcare providers.
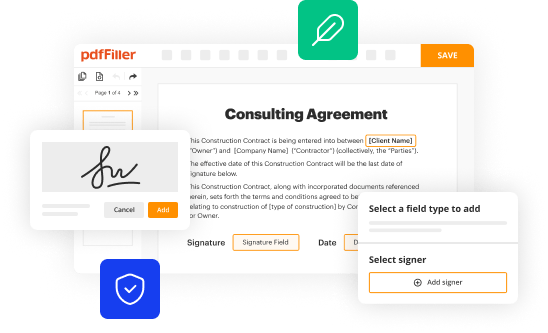
Enhancing document management with pdfFiller
pdfFiller provides advanced document management features that simplify the process of creating, signing, and submitting coverage determination request forms. Collaboration is crucial when multiple healthcare providers or team members need to contribute to the document. With pdfFiller’s collaboration tools, users can share and edit forms in real-time, ensuring everyone involved stays aligned and updated.
Organizing documents efficiently helps avoid chaos and confusion. Users can categorize and store completed coverage determination requests for easy access, ensuring pertinent documents can be retrieved without hassle. Additionally, the advantage of cloud-based document management means that forms are accessible anytime and from anywhere, enhancing workflow efficiency for both individuals and teams.
Best practices for submitting coverage determination requests
Submitting coverage determination requests should be approached with thorough planning and attention to detail. Timeliness is key; the sooner you submit your request following a treatment recommendation, the better the chances of receiving an approval in a timely manner. Having a proactive approach significantly reduces the risk of treatment delays.
Keeping detailed records is equally important. Document all communications with the insurance provider regarding your request, including calls and emails. Maintain records of the request itself, as this serves as a critical reference in case of disputes or follow-ups. Following up on your request is also crucial; checking in with the insurer can help speed up processing times.
Understanding your rights and options
Patients have the right to request a coverage determination, and understanding this right is essential for navigating the insurance process. If an individual finds themselves in a situation where their coverage request is denied, it’s crucial to know the available options. Patients can appeal the denial, providing additional documentation or clarification on why the coverage should be granted. This process often requires a thorough review of the original request along with any additional evidence that may support the need for treatment.
Utilizing tools within pdfFiller can facilitate the appeals process as well. By organizing all related documents and communications in a singular platform, users can efficiently compile the necessary information to launch an effective appeal.
Leveraging pdfFiller features for enhanced document creation
To create a streamlined and efficient experience when completing a coverage determination request form, leveraging pdfFiller offers a range of interactive tools. Users can access templates tailored for various coverage determination requests, ensuring they fill the forms accurately, adhering to all required specifications.
Additionally, the benefits of using eSigning allow for a legally compliant and smooth signing process, negating the need for physical signatures that can slow down the submission process. This electronic approach to document management ensures that users can manage their forms effectively, reducing time and hassle. Lastly, pdfFiller's customization options allow users to modify templates to fit their unique needs, making it easier to provide all required information seamlessly.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I send coverage determination request form for eSignature?
How do I complete coverage determination request form online?
How do I complete coverage determination request form on an iOS device?
What is coverage determination request form?
Who is required to file coverage determination request form?
How to fill out coverage determination request form?
What is the purpose of coverage determination request form?
What information must be reported on coverage determination request form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.