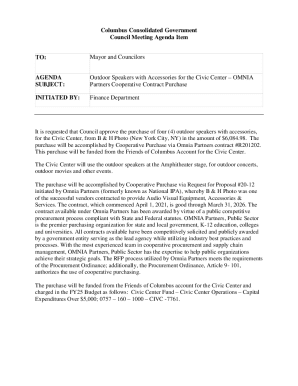
Get the free Fintepla Prior Authorization Request Form
Get, Create, Make and Sign fintepla prior authorization request



Editing fintepla prior authorization request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out fintepla prior authorization request

How to fill out fintepla prior authorization request
Who needs fintepla prior authorization request?
Understanding the Fintepla Prior Authorization Request Form
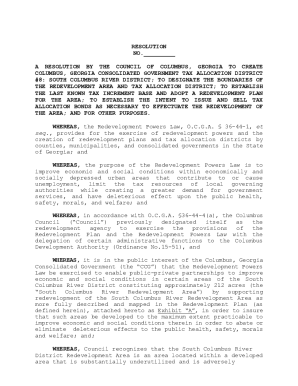
Understanding the Fintepla prior authorization process
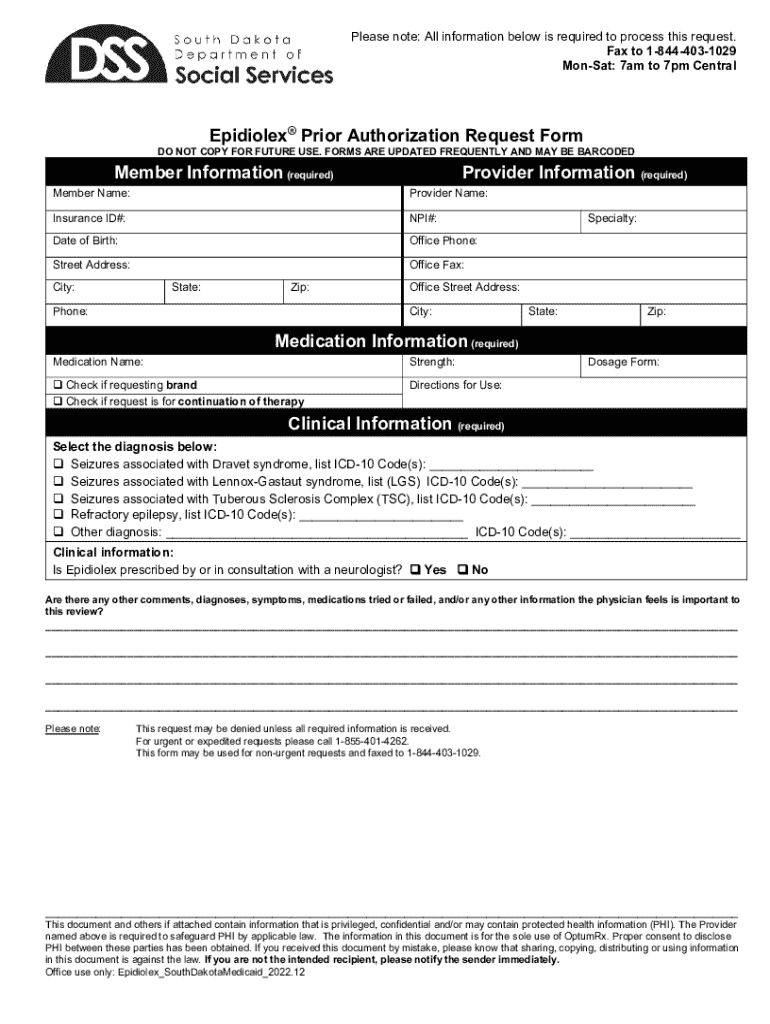
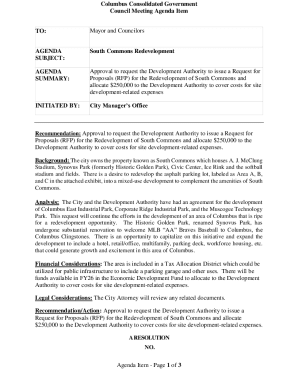
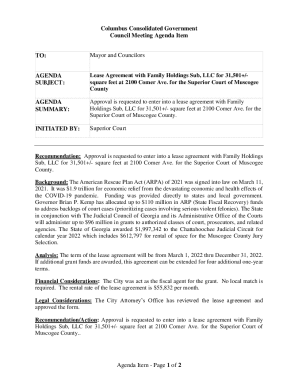
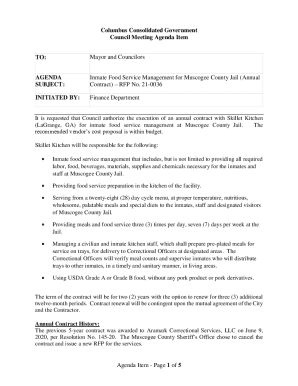
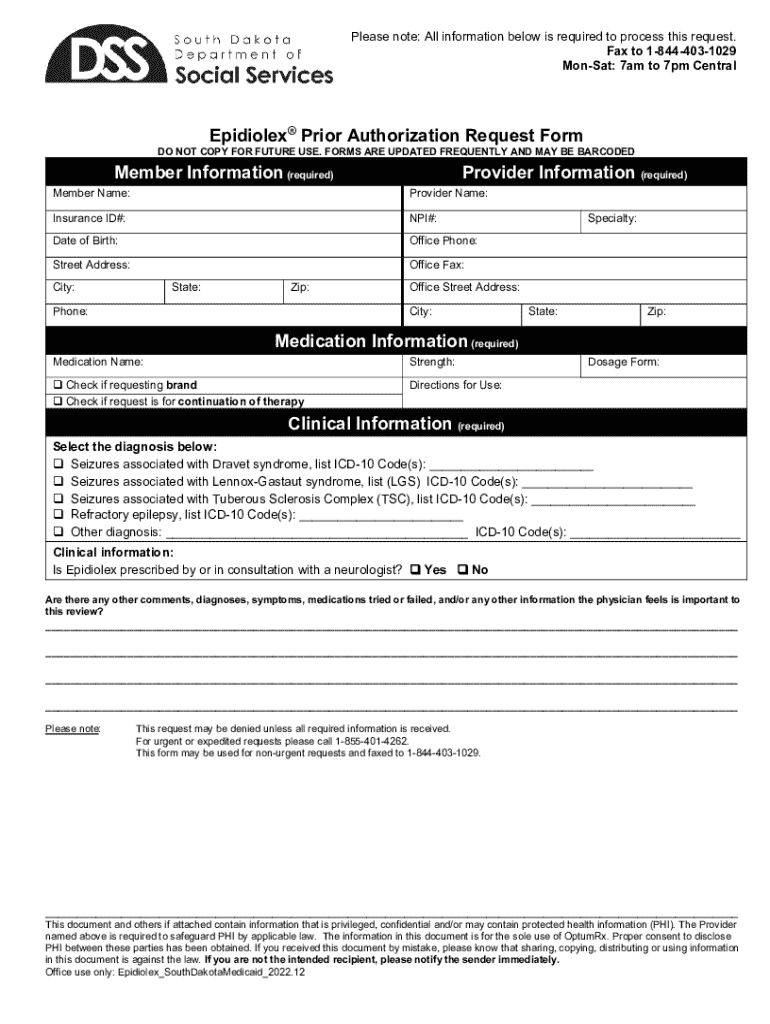
Fintepla, an oral solution formulated for the treatment of seizures associated with Dravet syndrome, requires a prior authorization request form to ensure appropriate use and reimbursement by insurance providers. Prior authorization serves as a critical step in confirming that treatments align with insurance guidelines, promoting both patient safety and effective use of medication within monetary constraints.
The importance of prior authorization can't be overstated. It ensures that patients receive the most appropriate medications while avoiding unnecessary healthcare costs. For individuals eager to access Fintepla, understanding who requires a prior authorization can significantly simplify the beginning of their treatment journey.
Key components of the Fintepla prior authorization request form
Completing the Fintepla prior authorization request form accurately is crucial for successful approval. The form requires essential information that helps convey the patient's needs, the prescribing physician's credentials, and the rationale for medication choice.
For starters, the patient information section should include basic details such as the full name, date of birth, and insurance information. Next, specific details about the prescribing physician, including their contact information and medical license number, are necessary to validate the prescriber’s authority.
Medication-specific information is equally vital, detailing the prescribed dosage and any relevant treatment history. Additionally, clear justification for medication use must be provided, comprising supporting diagnoses and any related medical history that underscores the need for Fintepla treatment.
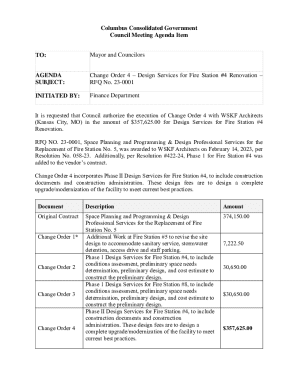
Step-by-step guide to completing the Fintepla prior authorization request form
Completing the Fintepla prior authorization request form can seem daunting, but breaking it down into manageable steps simplifies the process. First, gather all required information before starting the form. This preparation includes ensuring you have the patient’s insurance information and clinical history readily available.
Next, begin by filling out the patient information accurately. Privacy considerations are paramount here, and you should ensure that personal details are handled with care. Follow this by including the prescribing physician's information, ensuring that any required signatures are obtained.
Adding clinical justification is perhaps the most crucial part of the process. Document the medical necessity for Fintepla by detailing the supporting diagnosis, any relevant medical history, and the expected benefits of using this medication over alternatives. Proper documentation significantly eases the approval path.
Tips for ensuring a successful submission
Submitting a Fintepla prior authorization request form correctly increases the likelihood of success. One common mistake is omitting crucial information—so, make sure to double-check all entries for accuracy, particularly patient demographics and clinical justifications.
Accurate information is vital not only for the initial submission but also for avoiding delays. Double-check that all required signatures are in place, as missing signatures can lead to denials. Effective communication with insurance providers is equally important; be prepared to follow up if information is missing or if additional documentation is required.
Submitting your Fintepla prior authorization request
Submitting the finished Fintepla prior authorization request form requires consideration of the available submission methods. Many insurers now provide online portals that allow for quick and efficient submission directly through their websites, which is often the preferred method for its speed.
However, traditional methods such as fax and standard mail are still valid options for those who prefer them or when online submission is not available. After submission, expect a confirmation of receipt from your insurance provider, granting reassurance that your request is in progress.
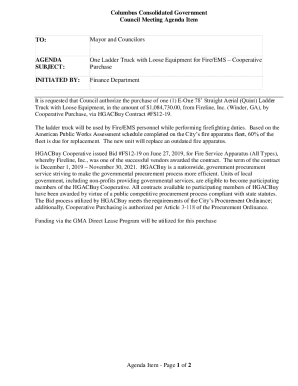
Addressing potential outcomes of your request
Understanding the possible outcomes after submitting your Fintepla prior authorization request is crucial. If your request is approved, the next steps involve coordinating with your pharmacy to start the medication. In the case of a denial, it’s imperative to know how to proceed.
Common reasons for denial include insufficient medical necessity documentation or failure to meet insurance criteria for coverage. Should your request be denied, filing an appeal becomes necessary. An appeal involves submitting additional documentation or clarifications to support the need for Fintepla effectively.
Tracking and managing your Fintepla authorization
Once a Fintepla authorization request has been submitted, managing and tracking the status is crucial. Utilizing pdfFiller can greatly enhance your document management, allowing you to keep excellent records of your request.
pdfFiller's tools can assist in collaboration with your healthcare team, enabling you to share updates and relevant documents seamlessly. Regular follow-ups with insurers should be a standard practice, as it helps to ensure that the process is moving along as expected and that any additional information requests are handled promptly.
FAQs about the Fintepla prior authorization request form
Frequently asked questions about the Fintepla prior authorization request form can assist patients and providers alike in better understanding the process. One common inquiry is about the duration of the authorization. Typically, a prior authorization last for a limited time, often ranging from 6 months to a year, depending on insurance provider policies.
Another significant question is whether an individual can appeal a denial independently. While it's possible, having assistance from healthcare professionals during this process can often yield better results, as they can provide appropriate documentation and medical insights.
Leveraging pdfFiller for efficient document management
Utilizing pdfFiller offers a seamless experience in managing your Fintepla prior authorization request form. The editing and collaboration features mean you can work on the document with your healthcare team and ensure everything is correct before submission.
Beyond this, pdfFiller’s eSigning capabilities expedite the approval process, enabling faster turnaround times. The platform ensures security and compliance in your document management, allowing you to focus more on your health rather than paperwork.
Final notes
Navigating the Fintepla prior authorization request form process can feel overwhelming, but it's essential to remain proactive throughout. Patients and caregivers should advocate for their health needs, ensuring that documentation is complete and accurate to facilitate access to necessary treatments.
Understanding how to utilize resources like pdfFiller not only helps in managing the submission process but also alleviates some of the stress associated with dealing with insurance providers. Remember, you’re not alone in this journey—support and information are available to help you every step of the way.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I modify fintepla prior authorization request without leaving Google Drive?
How do I complete fintepla prior authorization request online?
How do I fill out fintepla prior authorization request using my mobile device?
What is fintepla prior authorization request?
Who is required to file fintepla prior authorization request?
How to fill out fintepla prior authorization request?
What is the purpose of fintepla prior authorization request?
What information must be reported on fintepla prior authorization request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.