How To Fill Out Cobra Election Form
What is How to fill out cobra election form?
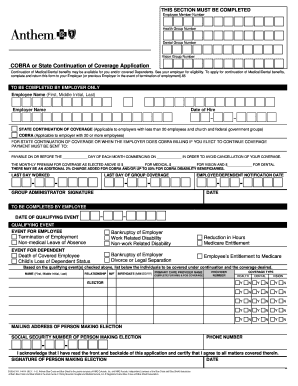
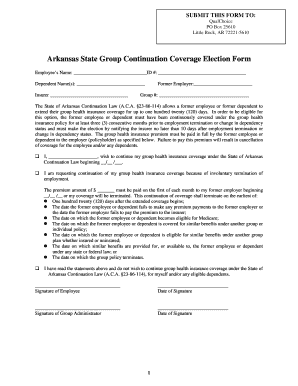
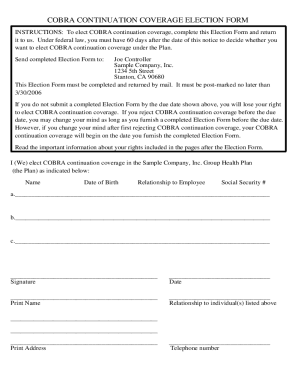
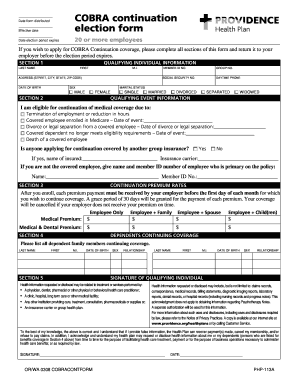
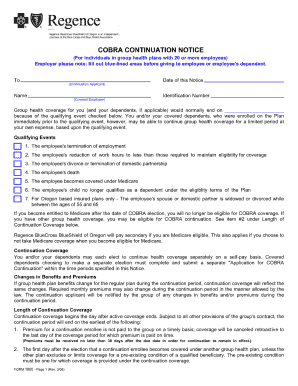
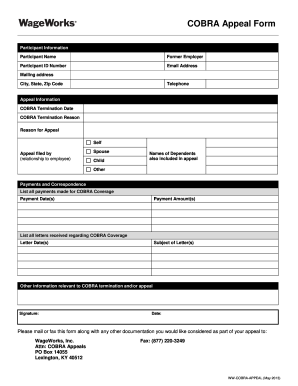
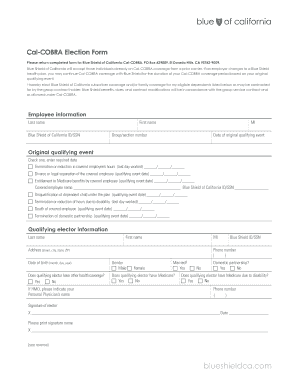
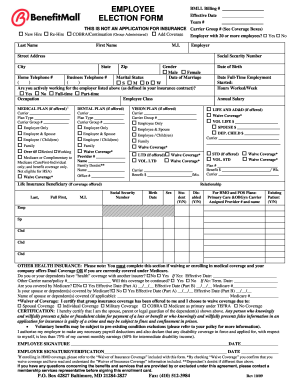
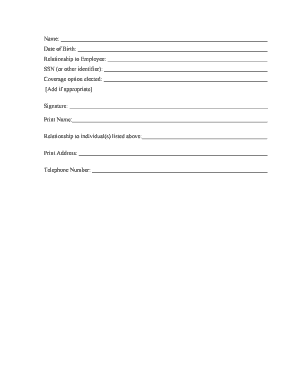
Filling out a COBRA election form is a crucial step for individuals who are eligible for continuing their health insurance coverage after experiencing a qualifying event, such as job loss. The form serves as a formal declaration of the decision to elect COBRA coverage, providing individuals with the option to maintain their insurance benefits for a certain period.
What are the types of How to fill out cobra election form?
There are typically two main types of COBRA election forms that individuals may encounter: the initial election form and the open enrollment election form. The initial election form is used when an individual first becomes eligible for COBRA coverage, while the open enrollment election form is utilized during specific periods where individuals can enroll in COBRA outside of their initial qualifying event.
How to complete How to fill out cobra election form
To successfully complete a COBRA election form, follow these steps:
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.