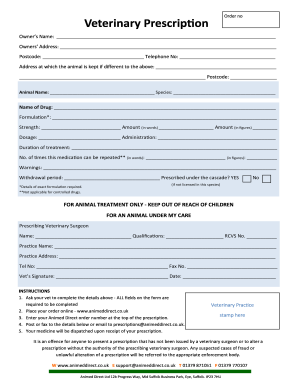
Veterinary Medical Record Example
What is Veterinary medical record example?
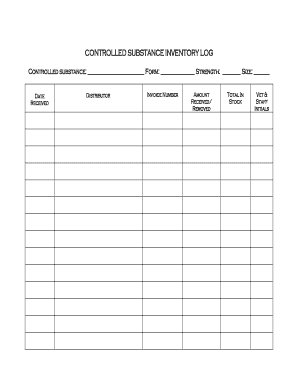
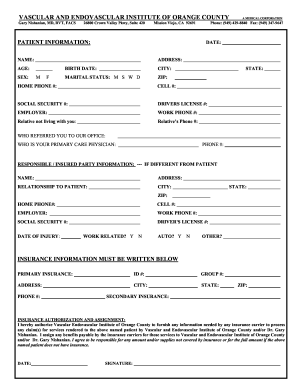
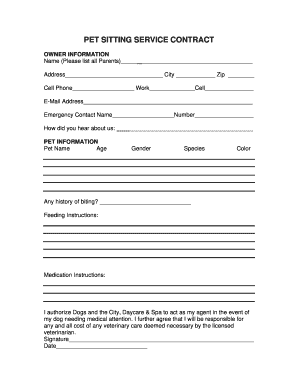
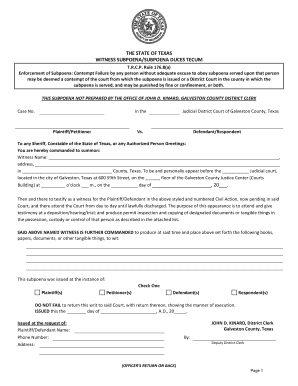
A veterinary medical record example is a comprehensive document that details a pet's health history, treatments, medications, vaccinations, and any other pertinent information related to their care. This record is essential for ensuring the well-being of the animal and providing proper treatment by veterinarians.
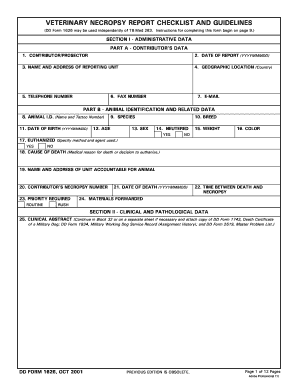
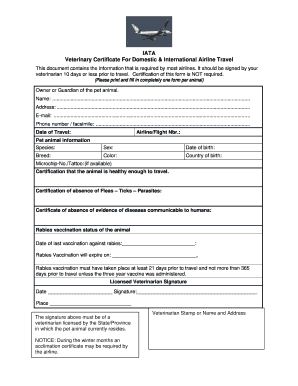
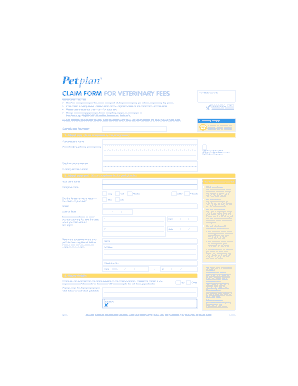
What are the types of Veterinary medical record examples?
There are various types of veterinary medical record examples that are used in different settings such as:
How to complete Veterinary medical record example
Completing a veterinary medical record example is crucial for maintaining accurate and up-to-date information on a pet's health. Here are some steps to follow:
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.