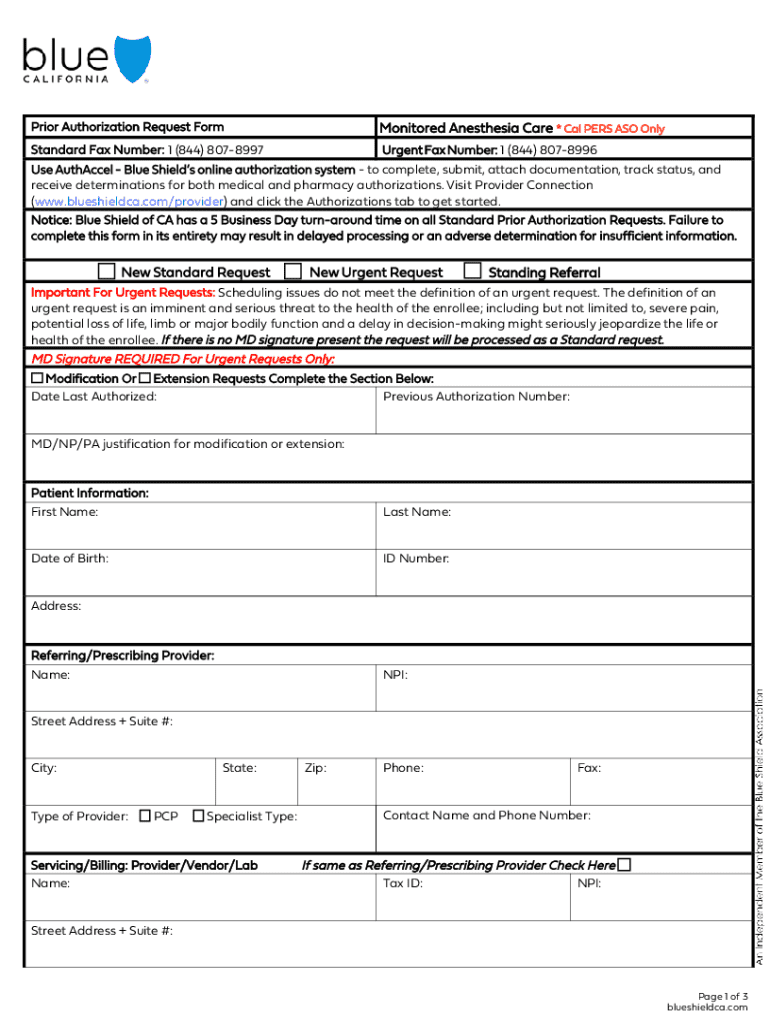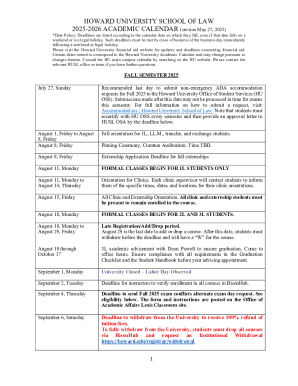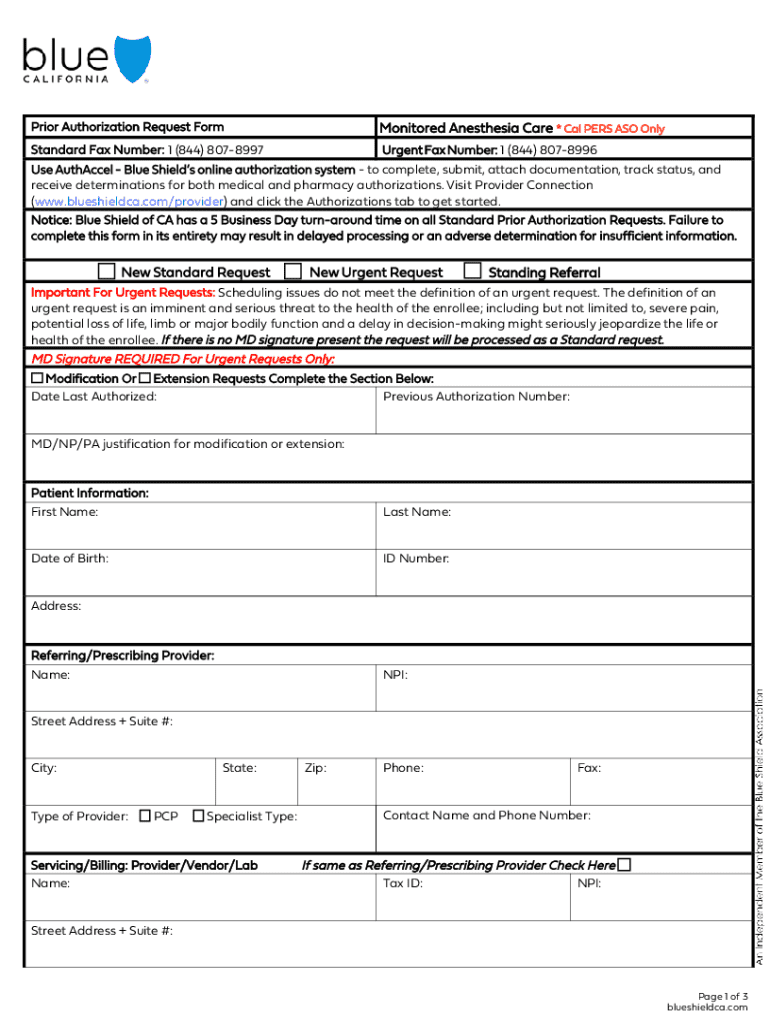
Get the free Prior Authorization Request Form Monitored Anesthesia ...
Get, Create, Make and Sign prior authorization request form



How to edit prior authorization request form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization request form

How to fill out prior authorization request form
Who needs prior authorization request form?
Your Complete Guide to the Prior Authorization Request Form
Understanding prior authorization
Prior authorization is a prerequisite for obtaining specific medical services or prescriptions where providers must obtain approval from the patient's health insurance company before the treatment is performed. This process is critical in the healthcare realm as it helps contain costs and ensures patients receive necessary treatments that align with insurer protocols.
The importance of prior authorization cannot be overstated; it serves a dual purpose—protecting patients from unnecessary procedures while allowing providers to verify that treatment stays within insurance guidelines. Stakeholders involved in this process include healthcare providers, patients, insurance companies, and sometimes pharmacists—each playing a critical role in accessing timely and appropriate medical care.
Common scenarios requiring prior authorization
Several treatments and services typically require prior authorization. These often include surgeries, expensive imaging tests like MRIs or CT scans, specialty medications, and certain outpatient procedures. Each insurance provider has its own list of services that require prior approval, impacting how healthcare is delivered.
For instance, patients with conditions such as cancer may need prior authorization for chemotherapy treatments or radiation therapies. Others with chronic illnesses like rheumatoid arthritis or multiple sclerosis may find themselves needing approvals for specialized medications. Notably, policies surrounding these approvals can vary significantly among different insurers, making familiarity with one's specific policy crucial.
Key components of the prior authorization request form
A prior authorization request form is integral for initiating the approval process. It requires specific details, generally divided into patient information, provider information, insurance plan details, and clear treatment descriptions.
Additionally, supporting documents often enhance the request's success, including relevant medical records, recommendations from specialists, and past diagnostic test results that substantiate the need for the proposed treatment.
Step-by-step instructions for completing the request form
Completing a prior authorization request form involves a systematic approach to ensure accuracy and completeness.
Editing and managing your prior authorization request form
The management of documents like the prior authorization request form can significantly impact the efficiency of the approval process. Utilizing tools like pdfFiller can streamline this task.
Moreover, the platform ensures secure sharing of documents, allowing healthcare teams to collaborate in real time, which is especially vital for cases requiring urgent approvals.
Monitoring the status of your prior authorization
Once a prior authorization request is submitted, monitoring its progress becomes essential. Patients can check with their insurance provider to understand where the request stands.
Being proactive in following up can sometimes expedite the approval process.
Best practices for a smooth prior authorization process
Patients can play a vital role in ensuring a seamless prior authorization process by preparing adequately for prescriptions and treatments. Here are key practices to consider:
Moreover, having a list of medications and treatment plans handy when discussing with insurers and healthcare providers can simplify discussions.
Advanced tips for teams managing multiple requests
For healthcare teams handling numerous prior authorization requests, efficiency is key. Here are advanced tips to improve your workflow:
Frequently asked questions about the prior authorization request form
Healthcare professionals and patients often have questions regarding the prior authorization request form. Addressing these queries is critical to facilitating a smoother experience.
Testimonials and case studies
Success stories can greatly enhance understanding of the prior authorization process. Users’ experiences reveal how a seamless process contributes to better patient care.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I send prior authorization request form for eSignature?
How do I fill out prior authorization request form using my mobile device?
How do I edit prior authorization request form on an iOS device?
What is prior authorization request form?
Who is required to file prior authorization request form?
How to fill out prior authorization request form?
What is the purpose of prior authorization request form?
What information must be reported on prior authorization request form?
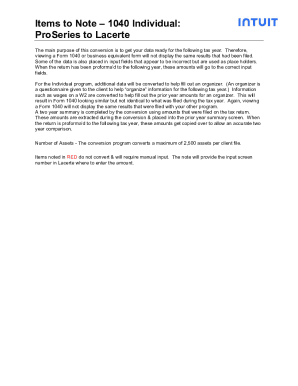
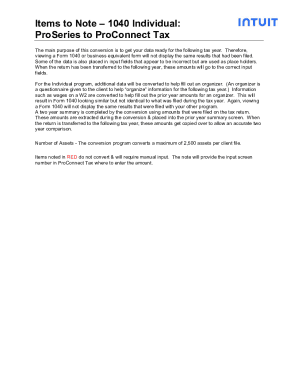
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.