Cobra Letter To Employee 2020 Template
What is Cobra letter to employee 2020 template?
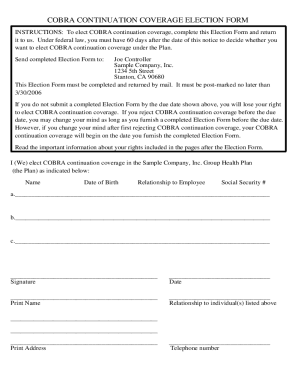
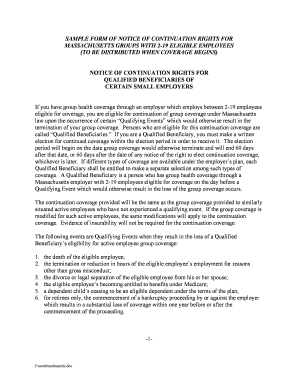
The Cobra letter to employee 2020 template is a standardized document that employers use to inform their employees about their rights to continue health insurance coverage under the Consolidated Omnibus Budget Reconciliation Act (COBRA) in 2020.
What are the types of Cobra letter to employee 2020 template?
There are mainly three types of Cobra letter to employee 2020 templates:
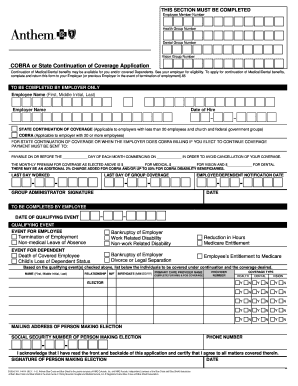
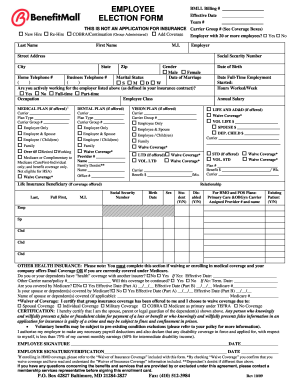
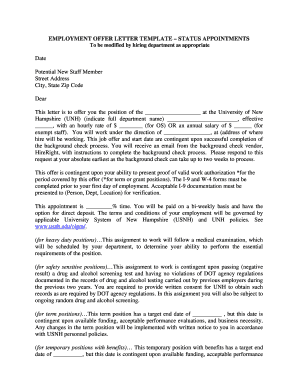
Standard COBRA notification letter template
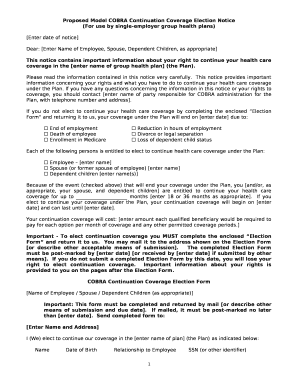
COBRA qualifying event letter template
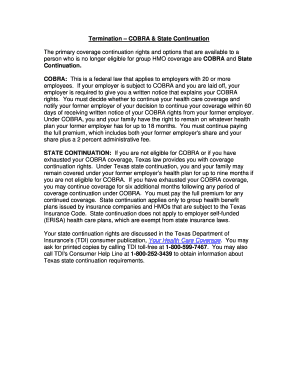
COBRA coverage termination letter template
How to complete Cobra letter to employee 2020 template
Completing the Cobra letter to employee 2020 template is a simple process that can be done in a few steps. Here's how:
01
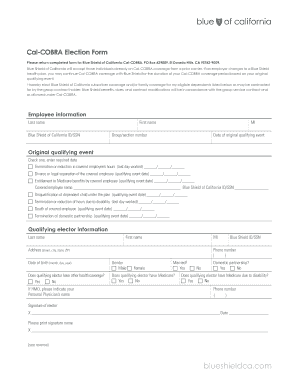
Fill in the relevant information about the employee and the employer
02
Specify the date of the qualifying event that makes the employee eligible for COBRA coverage
03
Include details about the COBRA coverage options available to the employee
pdfFiller is the go-to solution for creating, editing, and sharing documents online. With unlimited fillable templates and powerful editing tools, pdfFiller makes completing the Cobra letter to employee 2020 template a breeze.
Video Tutorial How to Fill Out Cobra letter to employee 2020 template
Thousands of positive reviews can’t be wrong
Read more or give pdfFiller a try to experience the benefits for yourself
Questions & answers
What is a COBRA continuation letter?
COBRA continuation coverage lets people who qualify keep their health insurance after their job ends, so it's not surprising that people who receive a COBRA notice might think they're job will soon be terminated. Getting a COBRA notice doesn't necessarily mean you'll be fired or laid off soon, though.
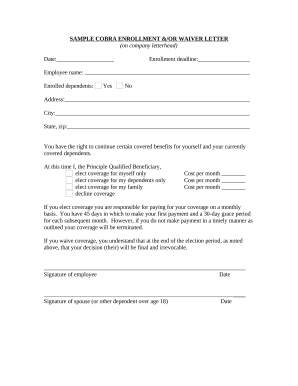
How do I write a COBRA termination letter?
The notice must explain the reason coverage has terminated, provide the date of termination and describe any rights the qualified beneficiary may have to elect alternative group or individual coverage, such as a conversion right (29 C.F.R. 2590.606-4(d)).
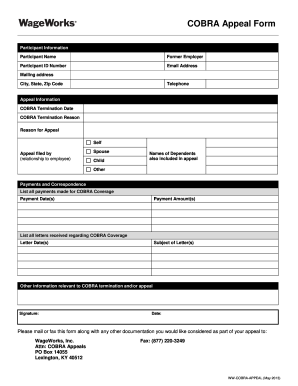
How do I get a COBRA termination letter?
When it's time to stop or cancel your coverage, you would need to make a request from the plan administrator to receive a letter of notice of COBRA termination. Typically, the COBRA Administrator is in the HR department or is a third-party administrator.
What are the rules for cancelling COBRA?
To cancel your COBRA plan you will need to notify your previous employer or the plan administrator in writing, requesting to terminate the insurance. The plan administrator is also who you've made your premium payments to.
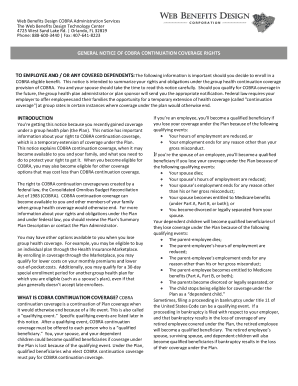
What is the COBRA general notice?
COBRA General Notice Group health plans must give each employee and spouse a general notice describing COBRA rights within the first 90 days of coverage. Group health plans can satisfy this requirement by including the general notice in the plan's SPD and giving it to the employee and spouse within this time limit.
What if my employer never sent COBRA information?
If your employer fails to notify the plan, you can contact the Department of Labor (DOL). The DOL fines companies that do not provide COBRA information within the proper time limits. You can also contact the benefits administrator at your previous company to ensure you receive the COBRA paperwork in time.