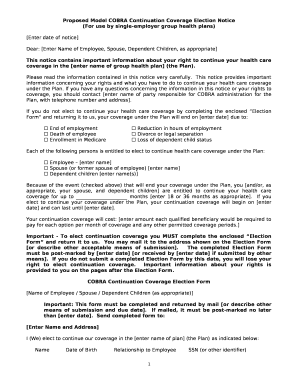
Cobra Continuation Coverage Election Notice California Employees
What is Cobra continuation coverage election notice California employees?
Cobra continuation coverage election notice is a notification provided to California employees who are eligible for continuing their health insurance coverage under the Consolidated Omnibus Budget Reconciliation Act (COBRA) after experiencing a qualifying event such as termination of employment.
What are the types of Cobra continuation coverage election notice California employees?
In California, employees may receive different types of Cobra continuation coverage election notices based on the qualifying event that triggered their eligibility. The types include:
How to complete Cobra continuation coverage election notice California employees
Completing your Cobra continuation coverage election notice in California is essential to maintain your health insurance benefits. Here are the steps to successfully complete the process:
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.