Cobra Open Enrollment - Page 2
What is Cobra open enrollment?
Cobra open enrollment is a period during which eligible individuals can sign up for continuation of their health insurance coverage after a qualifying event that would normally result in the loss of coverage.
What are the types of Cobra open enrollment?
There are generally two types of Cobra open enrollment: the initial enrollment period, which begins when coverage is initially lost, and the annual open enrollment period, which occurs each year during a specified timeframe.
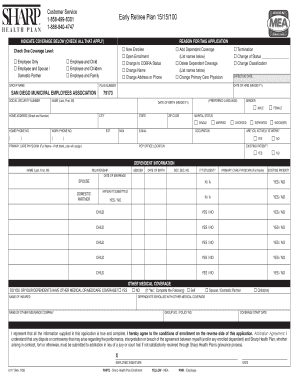
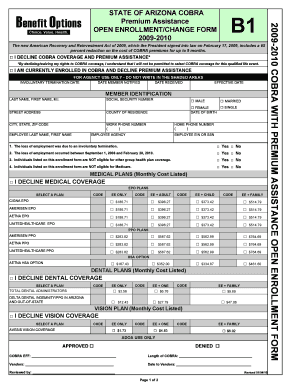
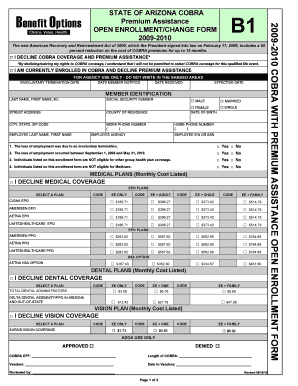
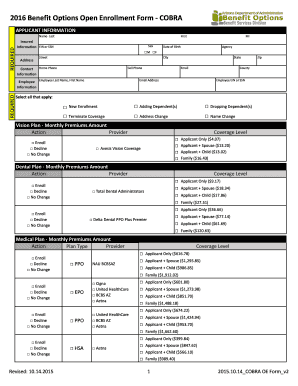
How to complete Cobra open enrollment
Completing Cobra open enrollment is a straightforward process that involves submitting the necessary paperwork and paying the required premiums on time. Here are some steps to help you through the process:
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.