Cobra Rules For Employers
What is Cobra rules for employers?
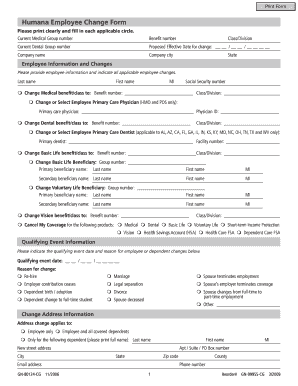
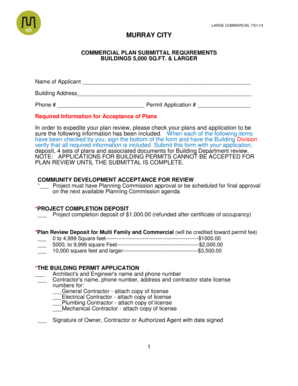
Cobra rules for employers refer to the regulations that require companies with 20 or more employees to provide continued health insurance coverage to employees and their families in the event of certain qualifying events such as the termination of employment or reduction in hours.
What are the types of Cobra rules for employers?
There are three main types of Cobra rules for employers:
Continuation Coverage
Notification Requirements
Premium Payment
How to complete Cobra rules for employers
To comply with Cobra rules for employers, follow these steps:
01
Provide the required notifications to employees and their beneficiaries about their rights under Cobra.
02
Collect timely premium payments from qualified beneficiaries.
03
Ensure that continuation coverage is offered and administered correctly.
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.
Video Tutorial How to Fill Out Cobra rules for employers
Thousands of positive reviews can’t be wrong
Read more or give pdfFiller a try to experience the benefits for yourself
Questions & answers
Can I use COBRA if I quit my job?
You have 60 days to enroll in COBRA once your employer-sponsored benefits end. You may even qualify if you quit your job or your hours were reduced. Other COBRA qualifying events include divorce from or death of the covered employee.
How long after leaving a job can you apply for COBRA?
When do I need to sign up for COBRA? You have 60 days from a “qualifying event” or the date your notice is mailed, whichever is later, to enroll in COBRA. A qualifying life event can be a job loss, divorce or death of your spouse, among others. Your former employer will send you details about how to sign up.
Does your insurance stop the day you quit?
Employers typically end your health insurance coverage on the effective day of your resignation or on the last day of the month in which you resigned. You should be able to find this information in your employee handbook.
What must employers have in order to be eligible for COBRA?
COBRA generally applies to all private-sector group health plans maintained by employers that have at least 20 employees on more than 50 percent of its typical business days in the previous calendar year.
What is the timeline for COBRA?
While COBRA is temporary, in most circumstances, you can stay on COBRA for 18 to 36 months.
Is COBRA 18 or 36 months?
You can collect COBRA benefits for up to 18 months. This may be extended to 36 months under certain circumstances. If your employer has 20 or more employees, it must follow COBRA rules. COBRA coverage follows a "qualifying event".