Humana Claim Reconsideration Form
What is humana claim reconsideration form?
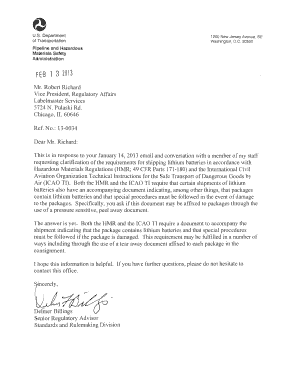
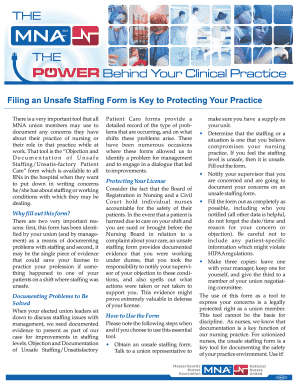
The humana claim reconsideration form is a document that allows individuals to request a review of a claim that has been denied or partially paid by Humana insurance. This form is used to provide additional information or evidence to support the reconsideration of the claim.
What are the types of humana claim reconsideration form?
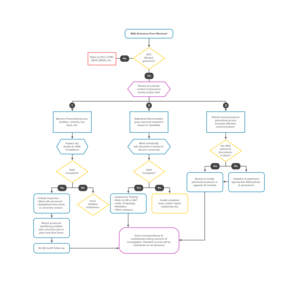
There are two main types of humana claim reconsideration forms: 1. Medical Necessity Review Form: This form is used when the denial is based on the claim not meeting the medical necessity criteria. 2. Administrative Appeal Form: This form is used when the denial is based on administrative reasons, such as incorrect coding or missing documentation.
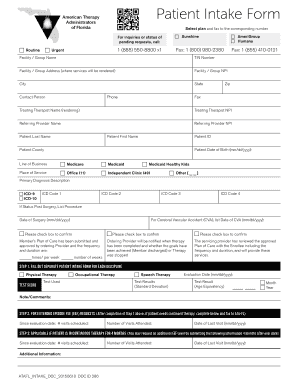
How to complete humana claim reconsideration form
To complete the humana claim reconsideration form, follow these steps: 1. Download the form from the Humana website or request a copy from your healthcare provider. 2. Fill in your personal information, including your name, address, and insurance policy details. 3. Provide a detailed explanation of why you believe the claim should be reconsidered. 4. Attach any supporting documents, such as medical records or invoices. 5. Sign and date the form. 6. Submit the form to the designated Humana claim reconsideration department.
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.