What is Unitedhealth Group International Claims Transmittal?
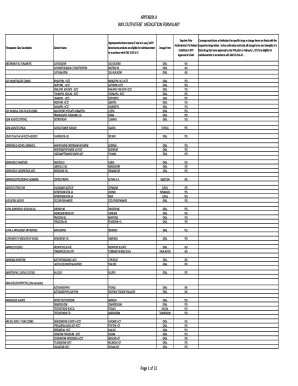
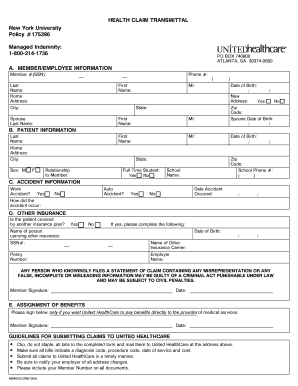
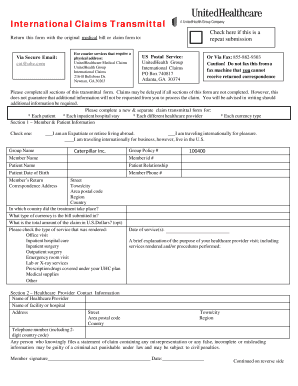
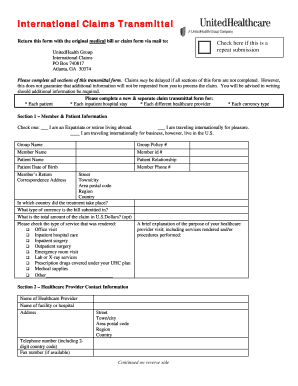
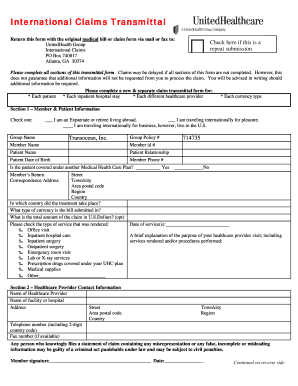
Unitedhealth Group International Claims Transmittal is a document used to submit claims for reimbursement of medical expenses incurred by international employees of Unitedhealth Group. It is an essential form that allows these employees to request compensation for their medical treatments and services received abroad.
What are the types of Unitedhealth Group International Claims Transmittal?
There are two main types of Unitedhealth Group International Claims Transmittal:
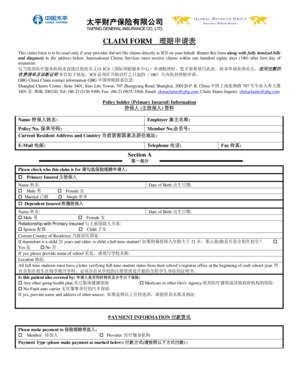
Individual Unitedhealth Group International Claims Transmittal: This type of transmittal is used by individual employees who have incurred medical expenses while traveling or residing abroad. They can submit their claims using this form.
Group Unitedhealth Group International Claims Transmittal: This type of transmittal is used by employers or organizations who have a group of international employees. It allows them to submit claims on behalf of multiple employees.
No matter which type of transmittal is used, both serve the purpose of facilitating the reimbursement process for international medical expenses.
How to complete Unitedhealth Group International Claims Transmittal
Completing the Unitedhealth Group International Claims Transmittal is a straightforward process. Follow these steps:
01
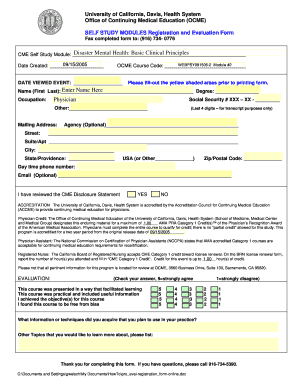
Download the Unitedhealth Group International Claims Transmittal form from the official website.
02
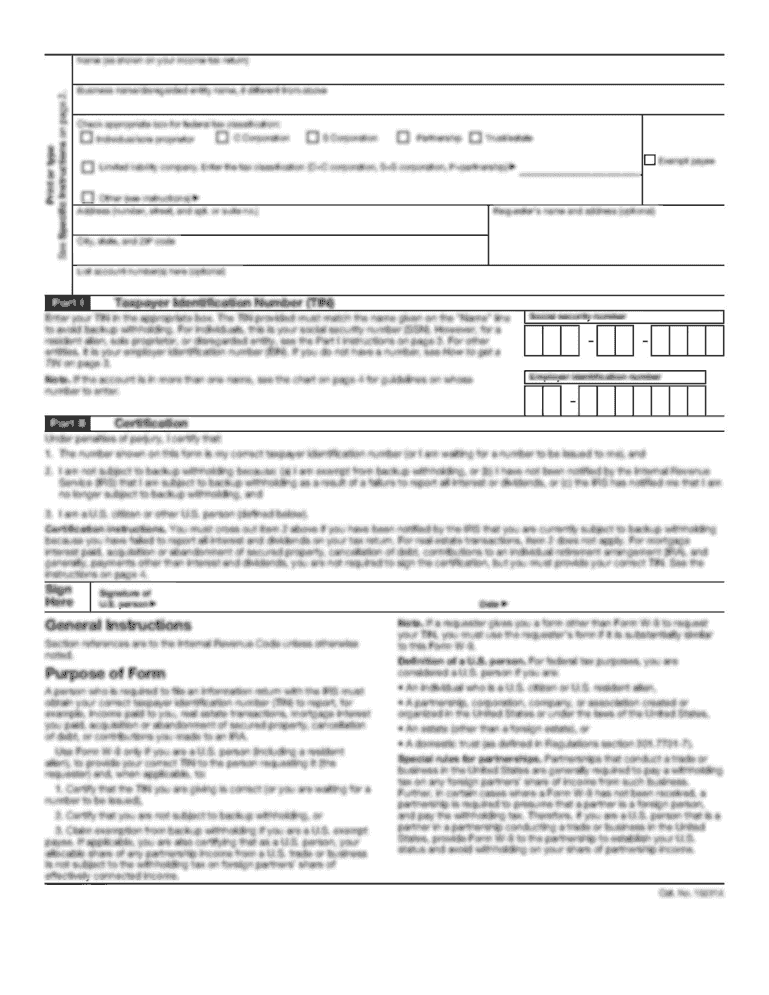
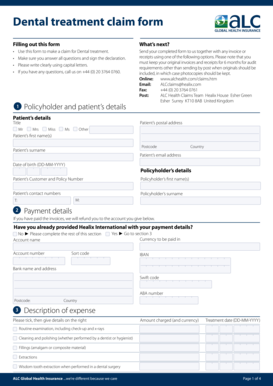
Provide the required personal and contact information, including name, address, and contact details.
03
Enter the details of the medical expenses incurred while traveling or residing abroad, including the dates and descriptions of treatments received.
04
Attach any supporting documents or receipts related to the medical expenses if required.
05
Review the completed form for accuracy and ensure all necessary information is provided.
06
Submit the completed Unitedhealth Group International Claims Transmittal form through the designated channel, either online or by mail.
07
Wait for the confirmation and processing of the claim. Be sure to keep a copy of the submitted form for your records.
With the help of pdfFiller, completing and submitting the Unitedhealth Group International Claims Transmittal form has never been easier. pdfFiller empowers users to create, edit, and share documents online, including unlimited fillable templates like the Unitedhealth Group International Claims Transmittal form. Its powerful editing tools ensure accuracy and efficiency in the completion process, making it the only PDF editor users need to get their documents done.