Get the free kentucky medicaid mco prior authorization request form
Show details
MAP 9 MCO 012016 1 Kentucky Medicaid MCO Prior Authorization Request Form Check the box of the MCO in which the member is enrolled Anthem BCBS Medicaid Coventry Cares/Aetna Better Health Human Resource
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign
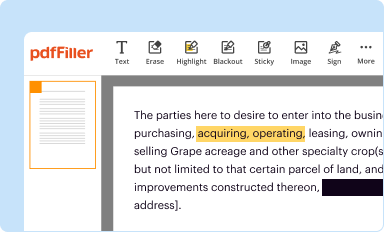
Edit your kentucky medicaid mco prior form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
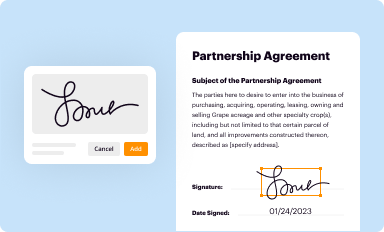
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
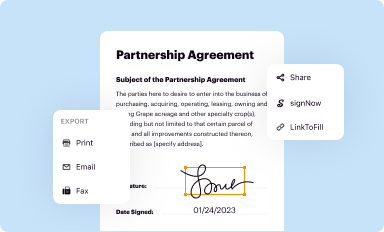
Share your form instantly
Email, fax, or share your kentucky medicaid mco prior form via URL. You can also download, print, or export forms to your preferred cloud storage service.
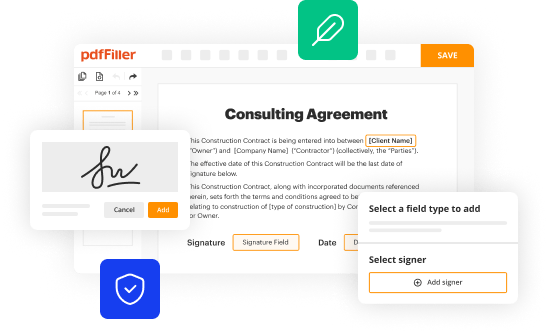
Editing kentucky medicaid mco prior authorization request form online
To use the services of a skilled PDF editor, follow these steps:
1
Log in to your account. Start Free Trial and register a profile if you don't have one.
2
Prepare a file. Use the Add New button. Then upload your file to the system from your device, importing it from internal mail, the cloud, or by adding its URL.
3
Edit ky medicaid prior authorization form. Rearrange and rotate pages, insert new and alter existing texts, add new objects, and take advantage of other helpful tools. Click Done to apply changes and return to your Dashboard. Go to the Documents tab to access merging, splitting, locking, or unlocking functions.
4
Save your file. Select it in the list of your records. Then, move the cursor to the right toolbar and choose one of the available exporting methods: save it in multiple formats, download it as a PDF, send it by email, or store it in the cloud.
With pdfFiller, it's always easy to deal with documents.
How to fill out kentucky medicaid mco prior
How to fill out Kentucky Medicaid MCO prior:
01
Gather all necessary information and documents such as personal information, income details, and medical history.
02
Access the Kentucky Medicaid website or contact the nearest Kentucky Medicaid office to obtain the required forms for MCO prior authorization.
03
Read the instructions carefully and fill out the forms accurately, providing all the requested information.
04
Pay attention to any specific guidelines or documentation needed for the particular medical service or medication you are seeking prior authorization for.
05
Ensure that you attach any supporting documents or medical records that are relevant to your request.
06
Double-check the completed forms for any errors or missing information, and make any necessary corrections.
07
Submit the filled-out forms along with any supporting documents to the appropriate Kentucky Medicaid office or the designated submission portal.
08
Keep a copy of the submitted forms and documents for your records.
Who needs Kentucky Medicaid MCO prior:
01
Individuals who are enrolled in the Kentucky Medicaid program and are utilizing Managed Care Organizations (MCOs) for their healthcare services.
02
Patients who require a specific medical service, treatment, procedure, or prescription medication that requires prior authorization from the MCO in order to be covered by Medicaid.
03
Healthcare providers who are requesting prior approval for their patients' medical services or medications to ensure that the costs are covered by Kentucky Medicaid.
Fill kentucky medicaid prior authorization form : Try Risk Free
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is kentucky medicaid mco prior?
Kentucky Medicaid MCO Prior refers to the prior authorization process required by Managed Care Organizations (MCOs) in the Kentucky Medicaid program. Prior authorization is a requirement for certain services, medications, or procedures to be approved and covered by Medicaid. The MCOs in Kentucky evaluate these requests and determine whether the requested services or medications are medically necessary and appropriate. Prior authorization helps to ensure cost-effective and appropriate use of Medicaid resources.
Who is required to file kentucky medicaid mco prior?
Health care providers in Kentucky who participate in the Medicaid Managed Care Organization (MCO) program are required to file prior authorization requests for certain medical services. This requirement applies to providers who offer services covered under the MCO program and wish to receive reimbursement for those services.
How to fill out kentucky medicaid mco prior?
To fill out the Kentucky Medicaid MCO prior authorization form, follow these steps:
1. Obtain the prior authorization form: You can usually get it from the Kentucky Medicaid website or your healthcare provider may provide you with a copy.
2. Fill in your personal information: Provide your full name, address, contact number, date of birth, and Medicaid ID number. Include the same information for the patient if it is different from yours.
3. Identify the MCO: Indicate the Managed Care Organization (MCO) you are enrolled in, as well as the MCO provider's name and address.
4. Provide healthcare provider information: Write down the name, address, and contact details of the healthcare provider who is requesting the prior authorization. Include their NPI (National Provider Identifier) if applicable.
5. Patient information: Input the patient's name, date of birth, Medicaid ID number, and any additional important details.
6. Describe the requested service/procedure: Explain the service or procedure that requires prior authorization. Provide specific details such as the diagnosis or indication for the requested service, proposed treatment plan, and any supporting medical documentation.
7. Attach supporting documents: Gather any relevant medical documentation, test results, or clinical notes that support the request. Include these as attachments along with the prior authorization form.
8. Sign and date the form: Ensure you sign and date the form to verify the accuracy of the information provided.
9. Submit the form: Send the completed prior authorization form, along with any necessary attachments, to the designated address listed on the form. It is recommended to keep a copy of the form for your records.
Note: It's important to review the instructions on the specific prior authorization form provided by your MCO or healthcare provider, as requirements may vary.
What is the purpose of kentucky medicaid mco prior?
The purpose of Kentucky Medicaid MCO (Managed Care Organization) prior authorization is to ensure that medically necessary services and treatments are covered before they are provided to Medicaid recipients. Prior authorization acts as a pre-approval process through which the MCO reviews the proposed medical services to determine if they meet the necessary criteria for coverage. This process helps control costs, improve efficiency, and prevent unnecessary or inappropriate utilization of healthcare services. It also ensures that Medicaid beneficiaries receive the appropriate and most cost-effective care.
What information must be reported on kentucky medicaid mco prior?
The information that must be reported on Kentucky Medicaid MCO prior includes:
1. Patient demographics: This includes the patient's name, address, date of birth, gender, and Medicaid identification number.
2. Insurance information: The patient's insurance information, including the name of the MCO and the Medicaid plan they are enrolled in.
3. Provider information: The name, address, and National Provider Identifier (NPI) number of the provider requesting prior authorization.
4. Service details: A detailed description of the requested service or procedure that requires prior authorization, including the diagnosis or reason for the service.
5. Supporting documentation: Any relevant medical records, test results, treatment plans, or other supporting documentation that justifies the medical necessity of the requested service.
6. Timeframe: The requested start and end dates for the service or procedure, if applicable.
7. Clinical justification: A statement explaining why the requested service is medically necessary and why alternative treatments or services would not be as effective.
8. Peer review information: If applicable, information from a peer-reviewed medical literature or authoritative medical opinions that support the requested service.
9. Signature: The signature and credentials of the provider requesting prior authorization.
It is important to note that the specific requirements for reporting on Kentucky Medicaid MCO prior authorization may vary, so providers should consult the guidelines and requirements of the specific MCO they are working with.
How can I edit kentucky medicaid mco prior authorization request form from Google Drive?
It is possible to significantly enhance your document management and form preparation by combining pdfFiller with Google Docs. This will allow you to generate papers, amend them, and sign them straight from your Google Drive. Use the add-on to convert your ky medicaid prior authorization form into a dynamic fillable form that can be managed and signed using any internet-connected device.
Where do I find pa form?
It's simple with pdfFiller, a full online document management tool. Access our huge online form collection (over 25M fillable forms are accessible) and find the kentucky medicaid mco prior authorization request form in seconds. Open it immediately and begin modifying it with powerful editing options.
Can I create an electronic signature for the kentucky medicaid mco prior authorization request form in Chrome?
You certainly can. You get not just a feature-rich PDF editor and fillable form builder with pdfFiller, but also a robust e-signature solution that you can add right to your Chrome browser. You may use our addon to produce a legally enforceable eSignature by typing, sketching, or photographing your signature with your webcam. Choose your preferred method and eSign your kentucky medicaid prior authorization form in minutes.
Fill out your kentucky medicaid mco prior online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Pa Form is not the form you're looking for?Search for another form here.
Keywords relevant to ky medicaid prior authorization form
Related to kentucky medicaid authorization form
If you believe that this page should be taken down, please follow our DMCA take down process
here
.