Get the free standardized prior authorization request form tufts
Show details
Massachusetts Administrative Simplification Collaborative Standardized Prior Authorization Request Form V1.1. November 2015. Standardized Prior ...
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign
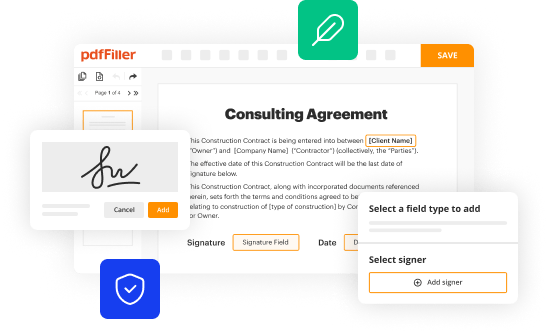
Edit your standardized prior authorization request form online
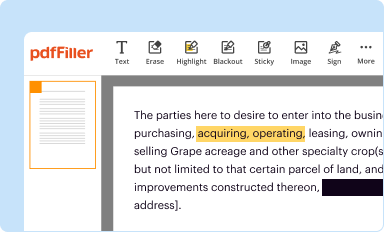
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
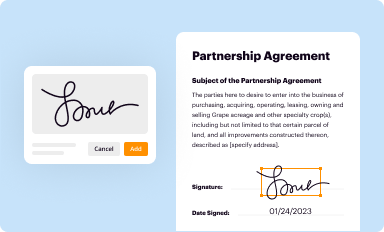
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
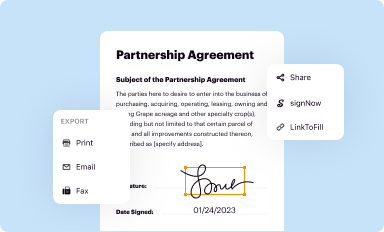
Share your form instantly
Email, fax, or share your standardized prior authorization request form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit standardized prior authorization request form tufts online
Follow the steps below to take advantage of the professional PDF editor:
1
Create an account. Begin by choosing Start Free Trial and, if you are a new user, establish a profile.
2
Prepare a file. Use the Add New button. Then upload your file to the system from your device, importing it from internal mail, the cloud, or by adding its URL.
3
Edit standard prior authorization form tufts. Add and change text, add new objects, move pages, add watermarks and page numbers, and more. Then click Done when you're done editing and go to the Documents tab to merge or split the file. If you want to lock or unlock the file, click the lock or unlock button.
4
Save your file. Select it from your list of records. Then, move your cursor to the right toolbar and choose one of the exporting options. You can save it in multiple formats, download it as a PDF, send it by email, or store it in the cloud, among other things.
With pdfFiller, it's always easy to work with documents. Check it out!
How to fill out standardized prior authorization request
How to fill out standardized prior authorization request:
01
Obtain the standardized prior authorization request form from your healthcare provider or insurance company.
02
Begin by filling in your personal information, including your full name, date of birth, address, and contact information.
03
Provide your insurance policy details, such as your policy number and the name of your insurance company.
04
Specify the healthcare service or treatment for which you are seeking prior authorization. Include the date you plan to receive the service or treatment, as well as any relevant medical codes or descriptions.
05
Attach any supporting documentation that may be required, such as medical records, test results, or physician's notes.
06
Sign and date the prior authorization request form to certify that the information provided is accurate and complete.
07
Submit the completed form and any accompanying documents to your healthcare provider or insurance company according to their preferred method (e.g., in person, by mail, or electronically).
Who needs standardized prior authorization request:
01
Individuals who have health insurance coverage and are seeking to obtain certain healthcare services or treatments may need to submit a standardized prior authorization request.
02
The requirement for a prior authorization request varies depending on the insurance plan and specific medical services. It is essential to check with your insurance company or healthcare provider to determine if prior authorization is necessary for a particular service or treatment.
03
Healthcare providers also play a significant role in requesting prior authorization on behalf of their patients, as they are responsible for submitting the necessary forms and supporting documentation to the insurance company.
Fill form : Try Risk Free
People Also Ask about standardized prior authorization request form tufts
Does Tufts require authorization?
Does Tufts CareLink require referrals?
Does Tufts follow Medicare guidelines?
How do I write a prior authorization request?
Does Tufts Medicare Preferred require prior authorization?
Does Tufts EPO require a referral?
What is the timeframe for a decision for a standard prior authorization request?
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is the purpose of standardized prior authorization request?
The purpose of a standardized prior authorization request is to provide a formal and structured process for healthcare providers to communicate with insurers or managed care organizations in order to obtain approval for certain medical treatments, procedures, medications, or services. Standardization helps streamline the prior authorization process and ensures consistency in the information required, reducing potential delays or errors.
By using standardized forms or formats for prior authorization requests, healthcare providers can efficiently provide all necessary clinical documentation, medical history, and supporting data needed to demonstrate the medical necessity and appropriateness of a particular treatment. This helps insurers make informed decisions regarding coverage, reimbursement, and utilization management.
Standardized prior authorization requests also aim to improve transparency and communication between healthcare providers and insurers, minimizing confusion or misinterpretation of request details. Additionally, they facilitate faster processing times and reduce administrative burdens for both parties involved, ultimately enhancing patient care coordination and access to appropriate treatments.
What is standardized prior authorization request?
A standardized prior authorization request refers to a uniform format or template used by healthcare providers or their representatives when requesting prior authorization for a specific medical service or treatment. This standardized form helps streamline the process by ensuring that all necessary information required for the authorization is filled out in a consistent and organized manner. It typically includes details such as patient demographics, medical necessity documentation, treatment codes, supporting clinical records, and any other pertinent information required by the insurance provider. By using a standardized prior authorization request, healthcare providers and insurers can expedite the process and reduce errors or delays in obtaining approval for healthcare services.
Who is required to file standardized prior authorization request?
Healthcare providers are required to file standardized prior authorization requests.
How to fill out standardized prior authorization request?
Filling out a standardized prior authorization request may vary depending on the specific form used by your healthcare provider or insurance company. However, here is a general guide on how to complete a prior authorization request:
1. Obtain the form: Contact your healthcare provider or insurance company to request the appropriate prior authorization form. You may be able to download it from their website or receive it via mail.
2. Personal information: Fill in your personal details, such as your name, address, phone number, date of birth, and insurance information. Ensure that all the information provided is accurate.
3. Patient information: If you are filling the form on behalf of someone else, such as a dependent, include their details, such as their name, date of birth, and relationship to you.
4. Healthcare provider information: Enter the name, address, and contact details of the healthcare provider who prescribed the medication, treatment, or procedure that requires prior authorization. Include their National Provider Identifier (NPI) if available.
5. Prescribed medication, treatment, or procedure: Clearly state the name of the medication, treatment, or procedure that requires prior authorization. Provide the diagnosis or reason for the request, along with any relevant supporting documentation, such as medical records or test results.
6. Insurance details: Include your insurance information, such as the policyholder's name, policy or group number, and the name of the insurance company. Attach a copy of your insurance card, if necessary.
7. Supporting documentation: If required, attach any supporting documentation that substantiates the medical necessity of the requested medication, treatment, or procedure. This may include medical records, test results, or a letter of medical necessity from your healthcare provider.
8. Explanation of benefits (EOB): If you have received an EOB for a previously denied service, attach it to the prior authorization request. This additional information may help support your case for approval.
9. Signature and date: Sign and date the request form to authorize the release of your medical information and to confirm that the information provided is true and accurate.
10. Submission: After completing the form, make a copy for your records and submit the original form to the designated address or fax number provided by your healthcare provider or insurance company. Be sure to keep track of the submission date for future reference.
Remember, this guide provides a general overview, and the specific requirements and instructions for completing a prior authorization form may vary. It's always a good idea to check with your healthcare provider or insurance company if you have any questions or need assistance in filling out the form correctly.
What information must be reported on standardized prior authorization request?
When submitting a standardized prior authorization request, the following information is typically required:
1. Patient Information: This includes the patient's name, date of birth, address, phone number, gender, and insurance details.
2. Provider Information: The requesting provider or prescribing physician's name, contact information, NPI/DEA number, and their specialty.
3. Medication Information: Details about the medication being requested, including the name, strength, dosage form, quantity, directions for use, and the National Drug Code (NDC) if available.
4. Clinical Information: The reason for the medication request, supporting diagnosis codes or ICD-10 codes, and any relevant medical history or clinical notes justifying the need for the requested medication.
5. Supporting Documentation: Any additional documentation that supports the request, such as lab results, imaging reports, progress notes, or treatment plans.
6. Insurance Authorization Number: If applicable, include the insurance policy or claim number for the patient.
7. Contact Information: The contact information for the person submitting the prior authorization request, in case there are any questions or follow-up required.
It is important to note that the specific requirements for prior authorization requests may vary depending on the insurance company, pharmacy benefit manager, or healthcare facility. It is always advisable to consult the specific guidelines or forms provided by the relevant organization when submitting a prior authorization request.
What is the penalty for the late filing of standardized prior authorization request?
The penalty for the late filing of standardized prior authorization requests can vary depending on the specific circumstances and the policies of the organization or insurance provider involved. Generally, late filing may result in the denial of the request, requiring the individual or healthcare provider to cover the cost of the authorized services themselves. Additionally, late filing could cause delays in treatment or medication approval, potentially affecting patient care. It is important to adhere to the specified filing deadlines to avoid these potential penalties.
How do I modify my standardized prior authorization request form tufts in Gmail?
The pdfFiller Gmail add-on lets you create, modify, fill out, and sign standard prior authorization form tufts and other documents directly in your email. Click here to get pdfFiller for Gmail. Eliminate tedious procedures and handle papers and eSignatures easily.
Where do I find tufts standard prior authorization form?
The pdfFiller premium subscription gives you access to a large library of fillable forms (over 25 million fillable templates) that you can download, fill out, print, and sign. In the library, you'll have no problem discovering state-specific tufts standardized prior authorization form and other forms. Find the template you want and tweak it with powerful editing tools.
How do I edit standard prior authorization form tufts straight from my smartphone?
Using pdfFiller's mobile-native applications for iOS and Android is the simplest method to edit documents on a mobile device. You may get them from the Apple App Store and Google Play, respectively. More information on the apps may be found here. Install the program and log in to begin editing standardized prior authorization request form tufts.
Fill out your standardized prior authorization request online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Tufts Standard Prior Authorization Form is not the form you're looking for?Search for another form here.
Keywords relevant to standardized prior authorization request form
Related to standardized prior authorization request form tufts
If you believe that this page should be taken down, please follow our DMCA take down process
here
.