Get the free Prior Authorization Request Prescriber Fax Glucagon-Like ...
Get, Create, Make and Sign prior authorization request prescriber



How to edit prior authorization request prescriber online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization request prescriber

How to fill out prior authorization request prescriber
Who needs prior authorization request prescriber?
Prior Authorization Request Prescriber Form - How-to Guide Long-Read
Understanding prior authorization requests
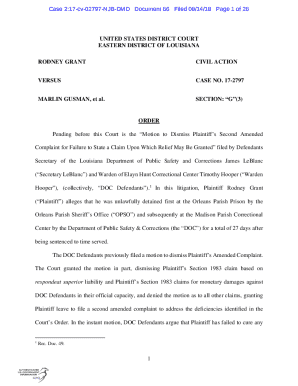
Prior authorization (PA) is a crucial component within the healthcare and insurance landscape, ensuring that specific medical services or treatments are covered by insurance providers. Essentially, it is a requirement that healthcare providers obtain approval from the insurance company before performing certain medical procedures or prescribing specific medications. This process helps control healthcare costs, verifies the necessity of treatments, and reduces unnecessary healthcare spending.
Understanding the importance of prior authorization is vital. It protects patients from unnecessary procedures while allowing insurers to manage their costs. Common scenarios where prior authorization is required include expensive specialty medications, inpatient admissions, and certain diagnostic services. The key stakeholders involved in this process include prescribers (the healthcare professionals), patients (the individuals receiving care), and insurance companies (the ones approving or denying requests).
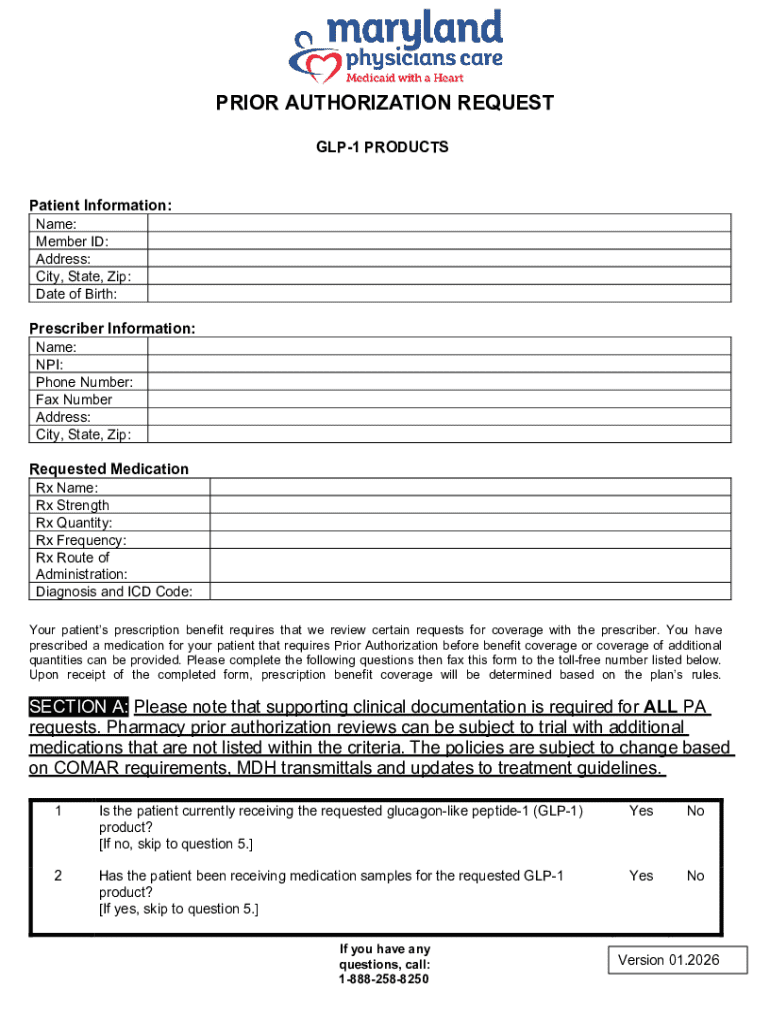
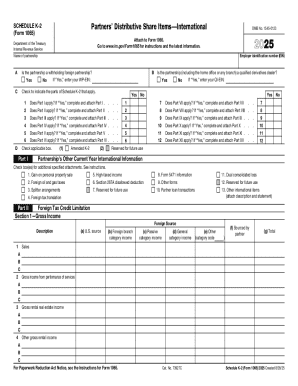
Overview of the prior authorization request prescriber form
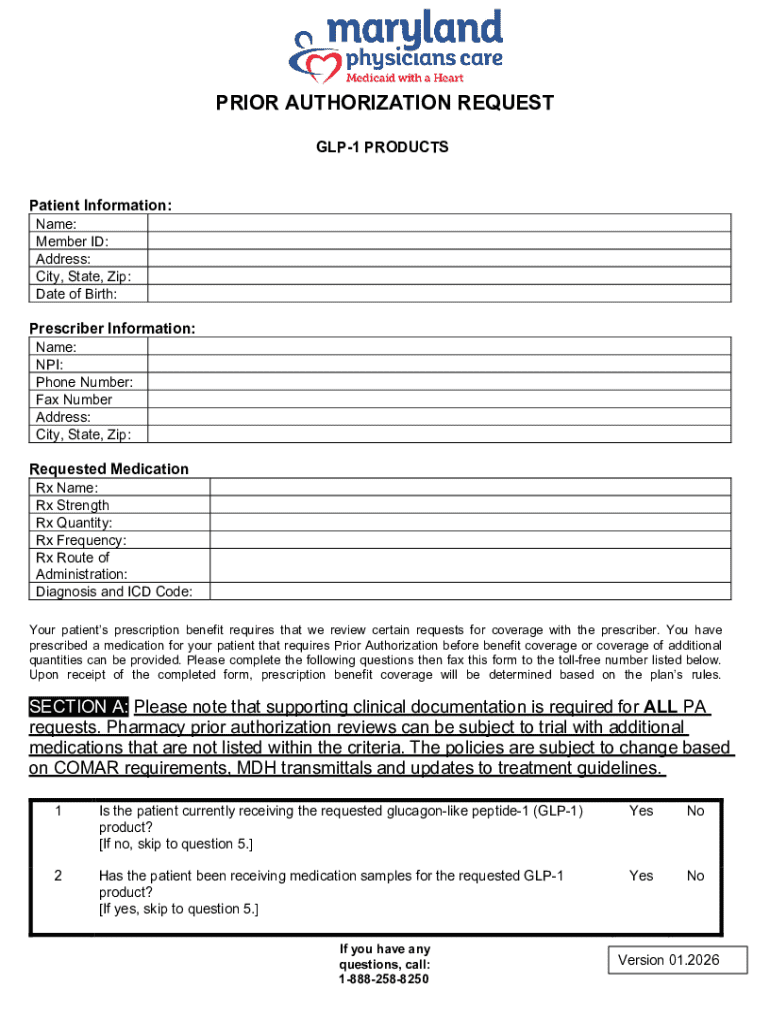
The prior authorization request prescriber form is designed to facilitate communication between healthcare providers and insurance companies. Its main purpose is to gather essential information regarding the patient's health status, the requested treatment, and the justification for its necessity. The benefits of utilizing this form include improving the speed and efficiency of approvals while ensuring compliance with insurance provider requirements.
This form streamlines the prior authorization process by providing structured sections that guide the prescriber in gathering the necessary information. Key information required on the form includes patient demographics, provider details, specifics of the medicine or service requested, and clinical justification that supports the need for the treatment. It's important to recognize that variations of the form exist based on the insurance provider, and prescribers must ensure they are using the correct version.
Accessing the prior authorization request prescriber form on pdfFiller
Finding the right prior authorization request prescriber form is essential for ensuring accurate submissions. pdfFiller offers an easy, streamlined way to access the correct documentation. Here’s a step-by-step guide to finding the form:
Using an up-to-date version of the form is crucial, as outdated forms may lead to delays or denials in the approval process.
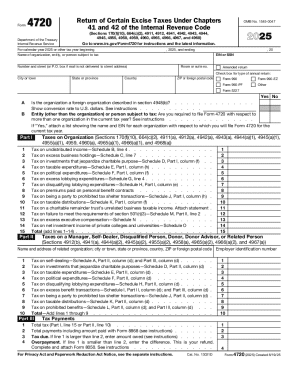
Filling out the prior authorization request prescriber form
Filling out the prior authorization request prescriber form accurately is essential for a successful submission. Each section has specific requirements that should be addressed carefully. Below are detailed instructions on how to complete each part of the form:
Avoid common mistakes such as leaving fields blank, providing generic justifications, or submitting an incomplete form, as these can result in processing delays or denials.
Editing and customizing the form with pdfFiller
pdfFiller provides robust editing tools that make it easy to customize the prior authorization request prescriber form to fit specific needs. Users can modify the form by adding or removing fields, inserting additional notes for clarity, or including attachments that support the request.
Additionally, pdfFiller’s interactive features facilitate collaboration among healthcare teams. Users can share the document with colleagues for input or confirmation. Managing different versions of the document is also seamless, allowing users to save their forms securely in the cloud for easy access and retrieval.
eSigning the prior authorization request form
eSigning the prior authorization request form is a critical step in the submission process. An electronic signature confirms the prescriber’s approval and intent to proceed with the request. It helps to ensure that the document is legally binding and can be processed efficiently by the insurance provider.
Using pdfFiller, eSigning is straightforward. Users can easily add their eSignature to the form with a simple click. Furthermore, once the form is signed, automatic notifications can be sent to other stakeholders involved, ensuring everyone is kept in the loop regarding the status of the authorization request.
Submitting the prior authorization request
Submitting the prior authorization request can be done through various methods, including physical mail or digital submission. The method chosen can depend on the specifications set by the patient's insurance provider and the urgency of the request.
It is essential to confirm the receipt of your submission by following up with the insurance company. Inquire about the expected timeline for approval to manage patient expectations effectively. Generally, the review period for approval can vary widely based on the complexity of the case and the insurance provider involved.
Following up on your prior authorization request
After submitting your prior authorization request, tracking the status of the approval is crucial for ensuring timely patient care. Regular follow-up is recommended to stay updated on the progress. Best practices involve establishing clear communication with the insurance provider, utilizing their customer service or patient services departments as needed.
In cases where a request is denied, it’s important to prepare for an appeal. Gathering additional documentation or evidence to support the necessity of the treatment can strengthen the case. Review the denial letter for specific reasons, as this will guide the appeal process effectively.
Best practices for efficient use of the prior authorization form
Adopting best practices can significantly enhance the efficiency of using the prior authorization request prescriber form. Maintaining thorough documentation and records of all requests, communications, and approvals is essential for streamlined processes.
Additionally, keeping updated with changes in insurance policies or requirements is critical. Health insurers often update their procedures, which can affect the prior authorization process. Leveraging pdfFiller for ongoing management of forms and documentation allows teams to stay organized and responsive to any changes in requirements.
Conclusion: empowering healthcare communication
Effective management of the prior authorization process is vital for improving patient care and ensuring that necessary treatments are provided without delay. By utilizing the prior authorization request prescriber form and the capabilities of pdfFiller, healthcare providers can navigate the complexities of insurance approvals more efficiently.
pdfFiller empowers users to seamlessly edit PDFs, eSign, collaborate, and manage documents from a single, cloud-based platform, thus enhancing the workflows of healthcare teams. Embracing these tools simplifies documentation processes and fosters better communication between stakeholders, ultimately benefiting patient outcomes.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I fill out prior authorization request prescriber using my mobile device?
Can I edit prior authorization request prescriber on an iOS device?
How do I fill out prior authorization request prescriber on an Android device?
What is prior authorization request prescriber?
Who is required to file prior authorization request prescriber?
How to fill out prior authorization request prescriber?
What is the purpose of prior authorization request prescriber?
What information must be reported on prior authorization request prescriber?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.