What is cigna provider forms?
Cigna provider forms are essential documents that healthcare providers need to complete in order to participate in Cigna's network and provide medical services to Cigna members. These forms help Cigna manage and update provider information, ensure smooth claim processing, and maintain accurate records. By filling out these forms, providers can ensure that they are compliant with Cigna's policies and regulations.
What are the types of cigna provider forms?
Cigna offers various types of provider forms based on the specific needs and requirements of healthcare providers. Some common types of Cigna provider forms include:
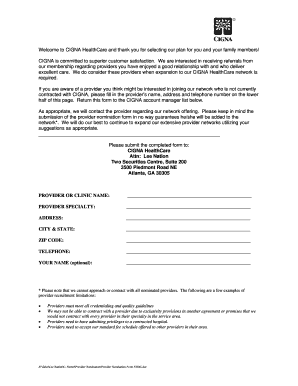
Provider Credentialing Application: This form is used by healthcare providers to apply for credentialing and become an in-network provider with Cigna.
Provider Contract Application: Providers use this form to apply for contracts with Cigna, which defines the terms and conditions of their participation in the network.
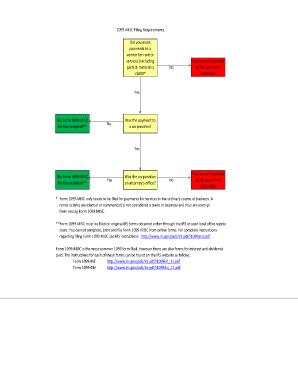
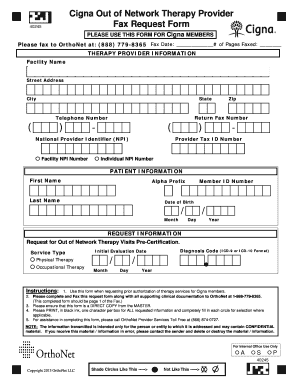
Claim Submission Form: This form is used by providers to submit claims for reimbursement of medical services provided to Cigna members.
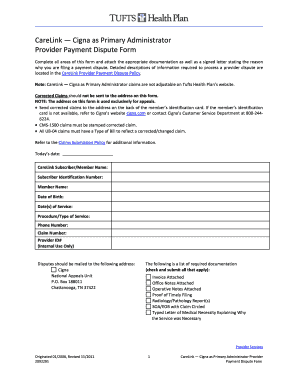
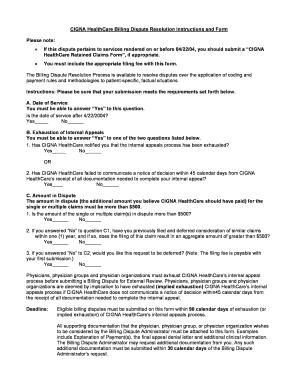
Appeal Form: In case of claim denial or dispute, providers can utilize this form to appeal the decision and request a review.
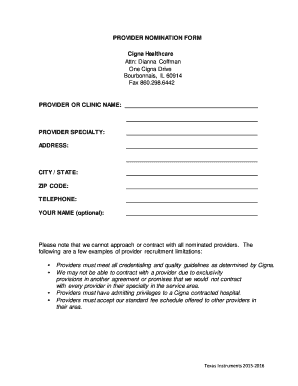
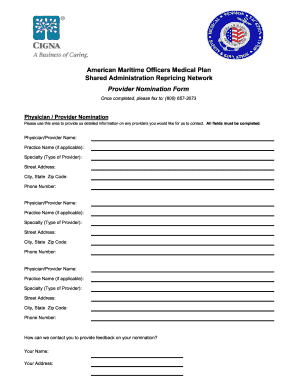
Provider Registration Form: This form is used to register new providers with Cigna and update their information.
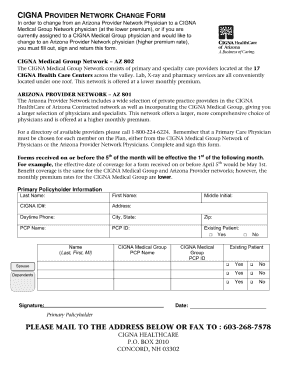
Provider Change Form: Providers can use this form to request changes to their existing information, such as address, contact details, or specialty.
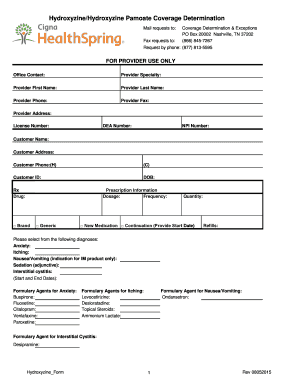
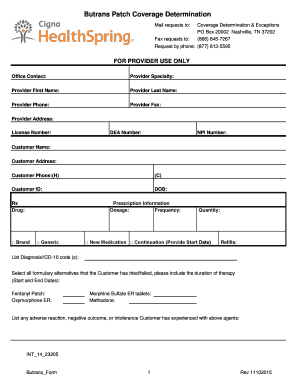
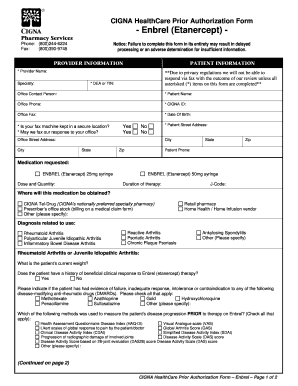
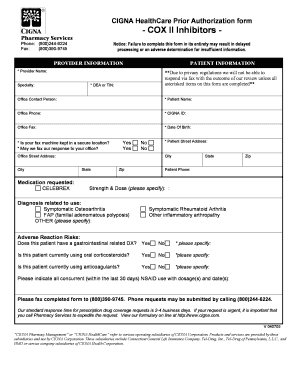
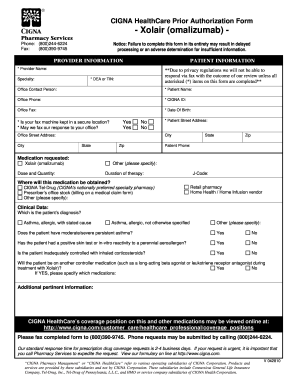
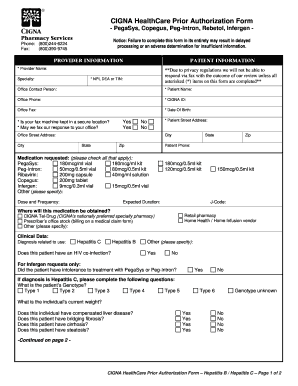
Authorization Request Form: This form is used for requesting prior authorization for certain medical procedures, treatments, or services.
Provider Directory Update Form: Providers can use this form to update their information in Cigna's provider directory to ensure accuracy and visibility for potential patients.
How to complete cigna provider forms
Completing Cigna provider forms is a straightforward process if you follow these steps:
01
Download the required form from the official Cigna website or obtain it directly from your Cigna representative.
02
Read the instructions carefully to understand the information and documents you need to provide.
03
Gather all the necessary documents, including your credentials, licenses, and any supporting records that may be required.
04
Fill out the form accurately and completely, ensuring that all required fields are filled in and all information provided is correct.
05
Double-check the form for any errors or missing information before submitting it.
06
Submit the completed form as instructed, either by mail, fax, or through an online portal if applicable.
07
Retain a copy of the completed form for your records.
By following these steps, healthcare providers can successfully complete Cigna provider forms and ensure smooth processing of their applications or claims.