Discharge Summary Template
Discharge Summary Template Definition and Tutorial
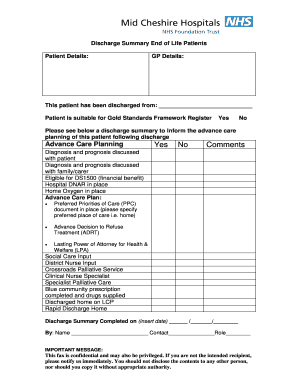
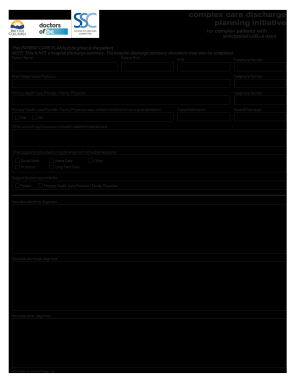
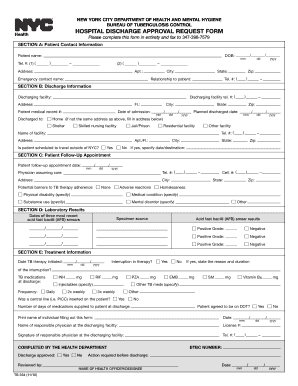
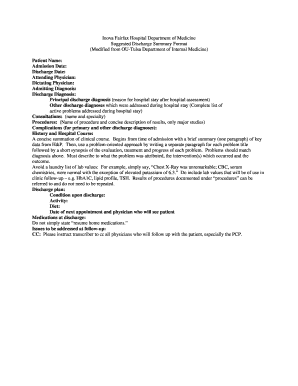
The discharge letter template is used when a medical facility releases a person after completing a treatment course, operation, etc. It is also used when patients change their physician. It is a brief description of the therapy recently received by the individual. It helps the doctor to understand a person's state of health and see what treatment should be applied. In most cases, the template is filled out with the use of medical terms that are not so easy to understand for an ordinary person (but are quite informative for doctors). The patient gets a copy, and the second document variant is sent to the general practitioner. Unlike the individual who gets the template right before leaving the hospital, the doctor may get a sample with a delay. Depending on the individual's state, the discharge may be minimal (if no care or little care is needed) or complex (for specialized or complicated care).
Components of the Medical Discharge Summary Letter
The discharge summary includes a basic set of information about the person admitted to the hospital and both the starting and finishing state. It includes the following information:
It is important to ask the doctor or nurse to provide a copy of the document before you leave the hospital.