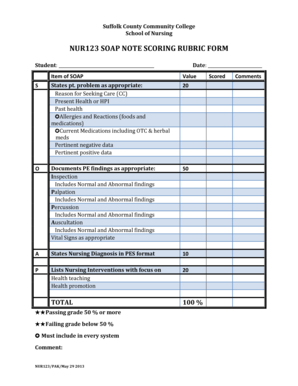
Nursing Soap Note Example
What is nursing soap note example?
A nursing soap note example is a documentation of a patient's condition, care, and progress during a hospital stay. It is a concise and organized way for nurses to record vital information about their patients, including medical history, symptoms, observations, and treatments.
What are the types of nursing soap note example?
There are several types of nursing soap note examples that can be used depending on the specific needs of the healthcare facility and the individual patient. Some common types include:
How to complete nursing soap note example
Completing a nursing soap note example requires careful observation, accurate documentation, and effective communication. Here are the steps to follow:
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.