Soap Note Example
What is a SOAP Note?
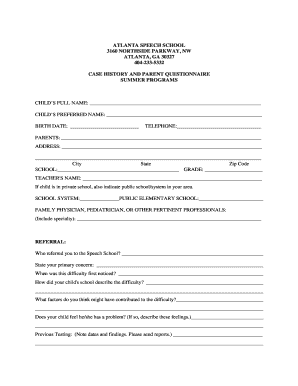
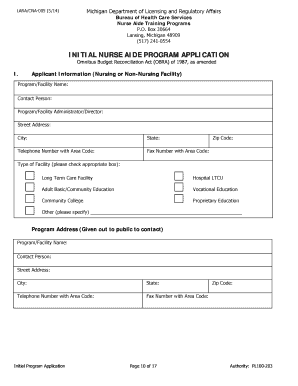
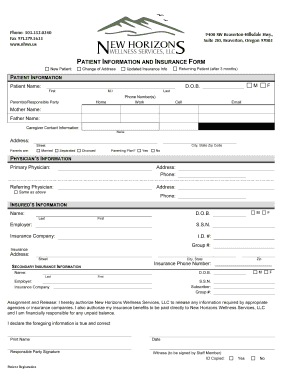
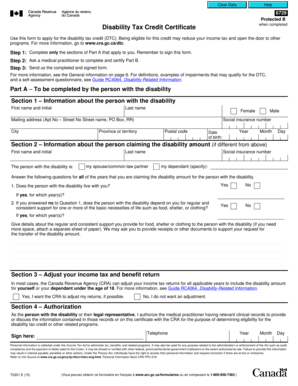
A patient’s chart is created by means of such documentation as a SOAP note template. It is used by health care workers. It includes four parts. Below you can see all of them:
This is a standard example of a SOAP note. Every medical worker must fill it out to record every step of the patient’s treatment process.
How to Fill Out a Soap Note
Generally, there are two available options. First of all, it is possible to write everything manually, printing out the document and using a pen for filling out all necessary fields.
Secondly, there is the option of downloading a PDF or Word format SOAP Note Template Form and simply typing all the information. You have access to many editing tools, which will greatly simplify the process of writing a soap note. Thus, you avoid all unnecessary paperwork, save time and can pay more attention to your patient.