Blue Cross Blue Shield Prescription Reimbursement Form - Page 2
What is blue cross blue shield prescription reimbursement form?
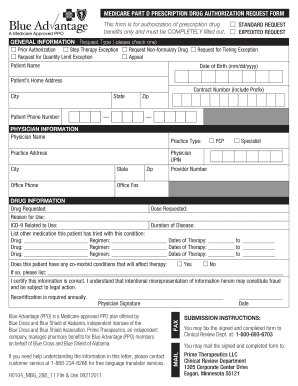
Blue Cross Blue Shield prescription reimbursement form is a document that allows policyholders to request reimbursement for prescription medications. This form is typically used when policyholders have paid for their prescriptions out of pocket and need to be reimbursed by their insurance provider. It requires detailed information about the prescription, including the name of the medication, the prescribing doctor, and the cost of the medication.
What are the types of blue cross blue shield prescription reimbursement form?
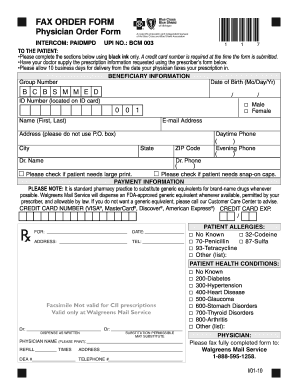
There are different types of Blue Cross Blue Shield prescription reimbursement forms depending on the specific insurance plan. Some common types include: 1. Standard Reimbursement Form: This form is used for general prescription reimbursement. 2. Specialty Medication Reimbursement Form: This form is used for reimbursement of specialty medications. 3. Mail Order Pharmacy Reimbursement Form: This form is used for reimbursement of prescriptions ordered through mail-order pharmacies. These forms may have slight variations in the required information, but the overall purpose is the same.
How to complete blue cross blue shield prescription reimbursement form
Completing the Blue Cross Blue Shield prescription reimbursement form is a straightforward process. Here is a step-by-step guide: 1. Obtain the form: You can usually download the form from the Blue Cross Blue Shield website or contact the customer service department to request a copy. 2. Fill in personal information: Provide your name, policy number, and contact information. This ensures that your reimbursement is credited to the correct policyholder. 3. Enter prescription details: Fill in the required information about the prescription, such as the name of the medication, dosage, prescribing doctor, and the cost of the medication. 4. Attach supporting documents: If required, include any supporting documentation such as receipts or invoices for the prescription. 5. Submit the form: Once you have completed the form and attached any necessary documents, submit it to the designated address or fax number provided. Make sure to keep a copy of the form and supporting documents for your records.
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.