Get the free humana credentialing status form
Show details
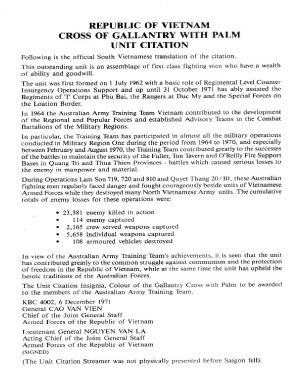
2010 Provider Reference Manual for physicians, health care professionals, facilities and ancillary providers 2010 Provider Reference Manual Table of Contents Section One: Oxford Contact Overview Contact
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign
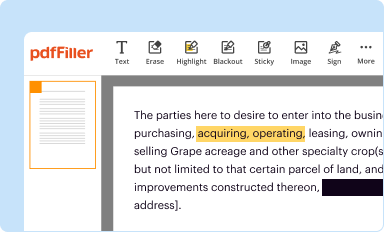
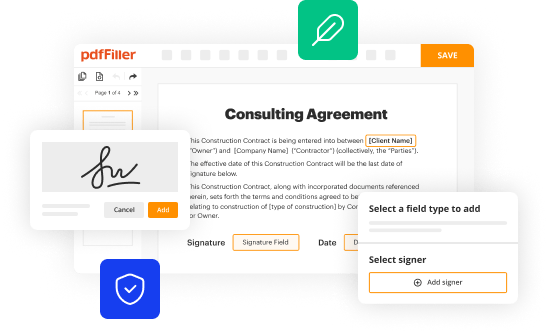
Edit your humana credentialing status form form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
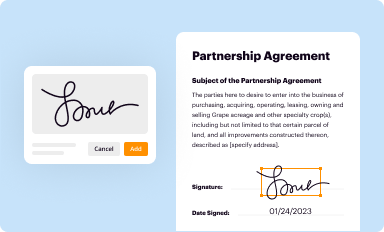
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
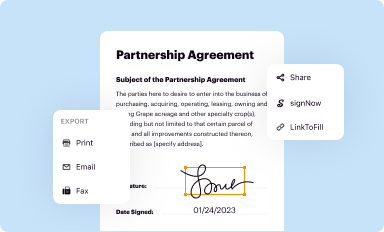
Share your form instantly
Email, fax, or share your humana credentialing status form form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit humana credentialing status online
To use our professional PDF editor, follow these steps:
1
Log in to your account. Click on Start Free Trial and sign up a profile if you don't have one yet.
2
Upload a file. Select Add New on your Dashboard and upload a file from your device or import it from the cloud, online, or internal mail. Then click Edit.
3
Edit humana provider enrollment application form. Rearrange and rotate pages, add new and changed texts, add new objects, and use other useful tools. When you're done, click Done. You can use the Documents tab to merge, split, lock, or unlock your files.
4
Get your file. Select the name of your file in the docs list and choose your preferred exporting method. You can download it as a PDF, save it in another format, send it by email, or transfer it to the cloud.
With pdfFiller, it's always easy to deal with documents. Try it right now
How to fill out humana credentialing status form
Filling out the humana credentialing status involves the following steps:
01
Gather all necessary information and documentation: Start by collecting all the required information, such as your personal details, contact information, education history, work experience, and any relevant certifications or licenses. Also, gather supporting documents, such as your resume, transcripts, and professional references.
02
Access the humana credentialing portal: Visit the official website of humana and log into the credentialing portal using your credentials. If you don't have an account, you may need to create one first.
03
Navigate to the credentialing status section: Once logged in, navigate to the section on the portal that specifically relates to credentialing status. It may be labeled as "Credentialing Application" or something similar.
04
Complete the application form: Fill out the application form accurately and thoroughly. Provide all the required information and upload the necessary documents as specified in the form. Double-check your entries for any errors or omissions before submitting.
05
Submit the application: After completing the form and ensuring all information is accurate, click on the submit button to send your application for humana credentialing status.
06
Await review and approval: After submission, your application will undergo a review process by humana. They will assess your qualifications, credentials, and other relevant factors. The time required for their decision may vary.
07
Receive the credentialing status: Once the review process is complete, you will receive notification of your humana credentialing status. If approved, you may be granted access to participate in humana's network and provide services to their members.
As for who needs humana credentialing status, it typically applies to healthcare professionals, such as physicians, dentists, nurse practitioners, physician assistants, and other healthcare providers. These professionals may need to obtain humana credentialing status to be eligible for contract participation with humana's network and to provide services to humana's insured members. However, it is important to consult with humana or check their specific requirements to determine if credentialing status is necessary for your particular situation.
Fill form : Try Risk Free
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is humana credentialing status?
Humana credentialing status refers to the process by which healthcare providers and practitioners apply to become part of Humana's network of approved providers. This involves submitting relevant documentation, such as medical licenses, certifications, and accreditation, for review by Humana's Credentialing Department. The status can be categorized as:
1. In-Network: This means that the healthcare provider successfully completed the credentialing process and is approved to provide services to Humana's members within their network.
2. Pending: This status indicates that the provider has submitted their application and is currently under review. The process can take some time, and the provider's status will be updated once the review is completed.
3. Out-of-Network: If a provider does not go through the credentialing process or their application is denied, they may be considered out-of-network and not eligible to provide services to Humana's members under their insurance plans.
It's important for providers to have an in-network credentialing status with Humana to ensure smooth reimbursement and accessibility for Humana members.
Who is required to file humana credentialing status?
The healthcare providers or medical professionals who are required to file Humana credentialing status are those who wish to become participating providers or join the provider network of Humana, an insurance company. This includes physicians, hospitals, nurses, dentists, specialists, and other healthcare providers. Credentialing is the process of verifying and evaluating their qualifications, background, and credentials to ensure that they meet the standards set by Humana.
What is the purpose of humana credentialing status?
The purpose of Humana credentialing status is to ensure that healthcare providers meet the necessary qualifications, standards, and regulatory requirements to participate in the Humana network. Credentialing is a comprehensive evaluation process conducted by Humana to verify a provider's education, training, experience, licensure, and other credentials. By maintaining a specific credentialing status with Humana, providers can gain access to network participation, which allows them to deliver services and receive reimbursement for their healthcare services to Humana beneficiaries. Overall, the purpose is to ensure that patients receive quality care from qualified and competent providers within the Humana network.
What information must be reported on humana credentialing status?
The information that must be reported on Humana credentialing status includes:
1. Personal Information: Name, address, contact information, and other identifying details of the healthcare provider or organization.
2. License and Certification: Details about the healthcare provider's license, certification, and registration, including the issuing authority and expiration dates.
3. Education and Training: Information about the healthcare provider's education, such as the name of the educational institution, degree obtained, and dates of attendance.
4. Work History: Details about the healthcare provider's previous work experience, including the name of the organization, position held, and dates of employment.
5. Malpractice History: Information about any professional liability claims, lawsuits, or settlements in which the healthcare provider has been involved.
6. References: Contact information for individuals who can provide reference checks or verify the healthcare provider's qualifications.
7. Insurance Coverage: Information about the healthcare provider's malpractice insurance coverage, including the insurance company and policy limits.
8. Medicare/Medicaid Enrollment: If applicable, details about the healthcare provider's enrollment in Medicare and/or Medicaid programs, including their National Provider Identifier (NPI) number.
9. Continuing Education: Information about the healthcare provider's participation in ongoing professional development activities or continuing education programs.
10. Accreditation and Quality Metrics: Details about any accreditations or quality metrics associated with the healthcare provider's practice, such as those related to patient care, safety, or outcomes.
It's important to note that the specific requirements for credentialing status reporting may vary based on Humana's policies and guidelines, as well as any applicable state or federal regulations.
How do I make edits in humana credentialing status without leaving Chrome?
Get and add pdfFiller Google Chrome Extension to your browser to edit, fill out and eSign your humana provider enrollment application form, which you can open in the editor directly from a Google search page in just one click. Execute your fillable documents from any internet-connected device without leaving Chrome.
How do I edit humana credentialing application on an iOS device?
Create, edit, and share humana provider credentialing application from your iOS smartphone with the pdfFiller mobile app. Installing it from the Apple Store takes only a few seconds. You may take advantage of a free trial and select a subscription that meets your needs.
How do I complete humana military provider credentialing application on an iOS device?
Get and install the pdfFiller application for iOS. Next, open the app and log in or create an account to get access to all of the solution’s editing features. To open your humana credentialing status, upload it from your device or cloud storage, or enter the document URL. After you complete all of the required fields within the document and eSign it (if that is needed), you can save it or share it with others.
Fill out your humana credentialing status form online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Humana Credentialing Application is not the form you're looking for?Search for another form here.
Keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.