NV FA-63 2017-2024 free printable template
Show details
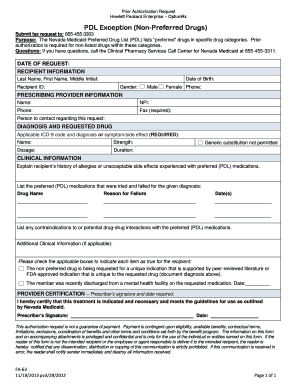
Prior Authorization Request Nevada Medicaid OptumRxPDL Exception (Preferred Drugs) Submit fax request to: 8554553303 Purpose: The Nevada Medicaid Preferred Drug List (PDL) lists preferred drugs in
pdfFiller is not affiliated with any government organization
Get, Create, Make and Sign
Edit your bcbs of ohio prior form online
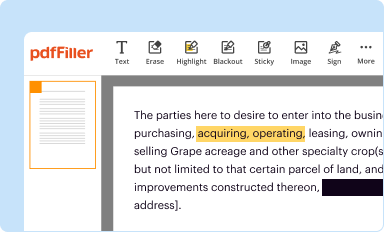
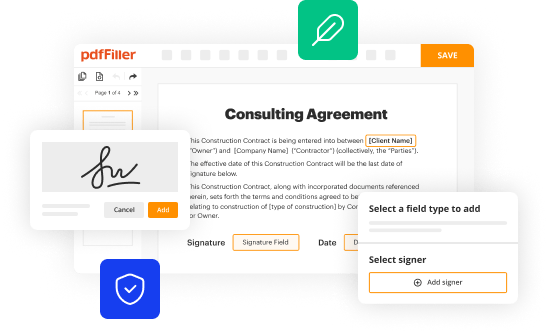
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
Share your form instantly
Email, fax, or share your bcbs of ohio prior form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit bcbs of ohio prior authorization form online
Here are the steps you need to follow to get started with our professional PDF editor:
1
Register the account. Begin by clicking Start Free Trial and create a profile if you are a new user.
2
Simply add a document. Select Add New from your Dashboard and import a file into the system by uploading it from your device or importing it via the cloud, online, or internal mail. Then click Begin editing.
3
Edit anthem bcbs ohio prior authorization form. Add and change text, add new objects, move pages, add watermarks and page numbers, and more. Then click Done when you're done editing and go to the Documents tab to merge or split the file. If you want to lock or unlock the file, click the lock or unlock button.
4
Save your file. Select it from your records list. Then, click the right toolbar and select one of the various exporting options: save in numerous formats, download as PDF, email, or cloud.
pdfFiller makes dealing with documents a breeze. Create an account to find out!
NV FA-63 Form Versions
Version
Form Popularity
Fillable & printabley
How to fill out bcbs of ohio prior
How to fill out BCBS of Ohio prior:
01
Download the BCBS of Ohio prior authorization form from their website.
02
Fill out your personal information accurately, including your name, address, and contact information.
03
Provide your BCBS of Ohio member ID number and policy number.
04
Clearly state the name of the medication or treatment for which you are seeking prior authorization.
05
Include the diagnosis or medical condition that justifies the need for the medication or treatment.
06
Attach any supporting documentation or medical records that may be necessary to substantiate your request.
07
Sign and date the form.
08
Submit the completed prior authorization form through the designated method specified by BCBS of Ohio, such as fax, mail, or online submission.
Who needs BCBS of Ohio prior:
01
BCBS of Ohio members who are seeking coverage for certain medications or treatments need to obtain prior authorization.
02
Healthcare providers or physicians who are prescribing medications or treatments that require prior authorization from BCBS of Ohio for their patients.
Fill 833 293 0659 : Try Risk Free
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is bcbs of ohio prior?
BCBS of Ohio Prior refers to the process of obtaining prior authorization from Blue Cross Blue Shield (BCBS) of Ohio before receiving certain medical services or treatments. Prior authorization is often required for specific procedures, medications, or therapies to ensure they are medically necessary, appropriate, and covered under the individual's insurance plan. The prior authorization process typically involves submitting a request and providing relevant medical documentation to BCBS of Ohio for review and approval before the service can be performed or the medication can be prescribed.
Who is required to file bcbs of ohio prior?
There is limited information available about "bcbs of Ohio prior." However, if you are referring to filing a claim with Blue Cross Blue Shield (BCBS) of Ohio, typically the policyholder or the healthcare provider (on behalf of the patient) is required to file a claim prior to receiving reimbursement for medical services. This applies to individuals covered under BCBS of Ohio insurance plans. It is advised to check with the insurance provider directly for specific details regarding claims filing requirements.
How to fill out bcbs of ohio prior?
To fill out a Blue Cross Blue Shield (BCBS) of Ohio prior authorization form, follow these steps:
1. Obtain the prior authorization form: You can usually download the form from the BCBS of Ohio website, obtain it from your healthcare provider, or contact the BCBS customer service for assistance.
2. Provide your personal information: Fill in your full name, address, phone number, and other required personal details as requested on the form.
3. Identify the patient information: Enter the patient's full name, date of birth, BCBS member ID number, and any other necessary information.
4. Specify the healthcare service or prescription drug: Indicate the specific procedure, treatment, or medication for which you are requesting prior authorization. Include the relevant diagnosis codes, medication details, and any other relevant information.
5. Attach supporting documentation: Attach any supporting medical records, test results, or relevant documentation that may be required to justify the medical necessity or effectiveness of the requested service or medication.
6. Complete the provider information: If you are not the healthcare provider submitting the request, provide the contact information and details of the referring or treating physician, including their name, address, phone number, and NPI number.
7. Sign and date the form: Sign and date the form to authorize the release of your medical information as required by BCBS of Ohio.
8. Submit the form: Send the completed prior authorization form, along with any additional documentation, to the designated BCBS of Ohio address. Be sure to follow any specific submission instructions mentioned on the form or provided by your healthcare provider.
Remember to keep a copy of the completed form and all attached documents for your reference. Additionally, it is advisable to follow up with BCBS of Ohio or your healthcare provider to ensure that your request for prior authorization has been received and processed.
What is the purpose of bcbs of ohio prior?
BCBS of Ohio prior refers to the prior authorization process of Blue Cross Blue Shield (BCBS) of Ohio, a health insurance company. The purpose of prior authorization is to determine if a specific medical service, treatment, or medication is medically necessary and meets the specific criteria defined by the insurance company before they provide coverage for it.
The prior authorization process is used to control healthcare costs, manage utilization, and ensure that patients receive appropriate and effective care. It helps insurance providers ensure that the requested procedure or medication is necessary, safe, and cost-effective, thereby preventing unnecessary treatments, reducing healthcare expenses, and improving the quality of care.
By requiring prior authorization, BCBS of Ohio ensures that medical resources are being utilized efficiently, while also ensuring that members receive the appropriate and necessary care they need.
What information must be reported on bcbs of ohio prior?
There is limited information available about BCBS of Ohio Prior, as it might refer to a specific form or process within BCBS of Ohio. However, typically, reporting requirements for health insurance prior authorization (prior) requests may include the following:
1. Patient Information: Name, date of birth, address, gender, and insurance identification number.
2. Provider Information: Name, address, contact information, and National Provider Identifier (NPI) number.
3. Procedure/Service Details: Description of the requested procedure, service, or treatment, including relevant CPT or HCPCS codes.
4. Diagnosis/Condition Information: Documentation of the patient's diagnosis or medical condition necessitating the procedure or service.
5. Supporting Documentation: Relevant medical records, test results, imaging reports, or any other information that supports the medical necessity of the requested procedure or service.
6. Treatment Plan: Description of the proposed treatment plan, outlining the recommended duration, frequency, and expected outcomes.
7. Name of Prescribing Physician: If requesting a specific medication, provide the name, dosage, and frequency prescribed.
8. Steps Already Taken: Information about any previous treatments, medications, or therapies attempted, along with their outcomes, if applicable.
9. Emergency/Urgent Request: In case of an urgent or emergent situation, additional information may be required to justify the immediate need for the requested procedure or service.
Please note that these are general guidelines for typical prior authorization requirements, and specific information may vary depending on the health insurance provider, plan, and the requested procedure or service. It is always best to consult with the insurance company directly or review their specific guidelines for accurate and up-to-date requirements.
How do I fill out bcbs of ohio prior authorization form using my mobile device?
Use the pdfFiller mobile app to fill out and sign anthem bcbs ohio prior authorization form on your phone or tablet. Visit our website to learn more about our mobile apps, how they work, and how to get started.
Can I edit bcbs of ohio prior authorization on an iOS device?
Create, modify, and share bcbs of ohio prior authorization phone number using the pdfFiller iOS app. Easy to install from the Apple Store. You may sign up for a free trial and then purchase a membership.
How do I fill out bcbs ohio prior authorization on an Android device?
Use the pdfFiller Android app to finish your bcbs ohio prior authorization form and other documents on your Android phone. The app has all the features you need to manage your documents, like editing content, eSigning, annotating, sharing files, and more. At any time, as long as there is an internet connection.
Fill out your bcbs of ohio prior online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Bcbs Of Ohio Prior Authorization is not the form you're looking for?Search for another form here.
Keywords relevant to anthem ohio prior authorization form
Related to bcbs ohio prior authorization
If you believe that this page should be taken down, please follow our DMCA take down process
here
.