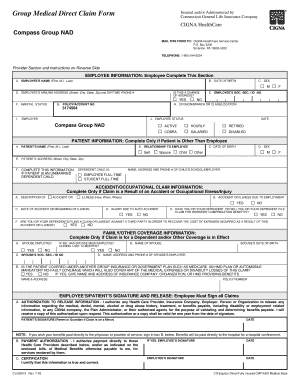
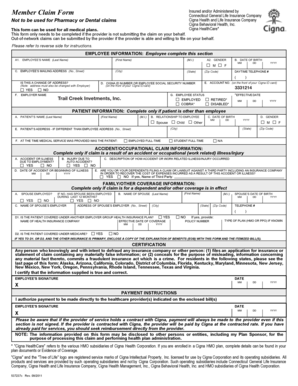
Cigna Medical Claim Form - Page 2
What is Cigna Medical Claim Form?
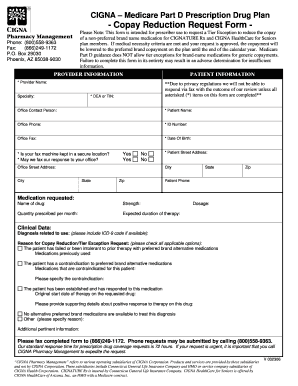
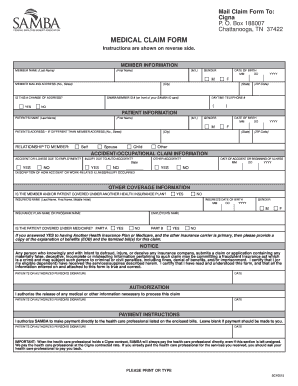
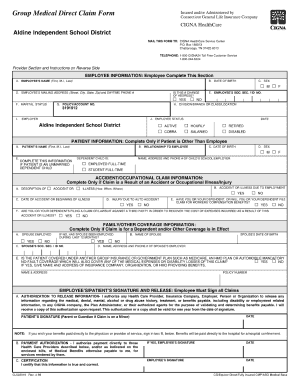
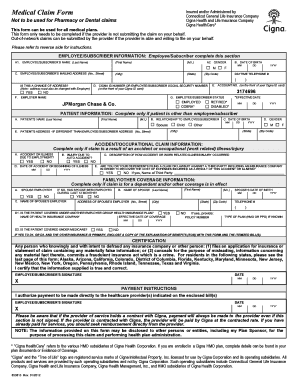
A Cigna Medical Claim Form is a document used to provide details about medical services or treatments that have been received by a patient. This form is typically filled out by the patient or their healthcare provider and serves as a way to request reimbursement from the insurance company.
What are the types of Cigna Medical Claim Form?
Cigna offers multiple types of Medical Claim Forms, tailored to specific needs. These forms include:
How to complete Cigna Medical Claim Form
Completing a Cigna Medical Claim Form is a straightforward process. Here are the steps to follow:
Empowering users to create, edit, and share documents online, pdfFiller is a leading platform that offers unlimited fillable templates and powerful editing tools. With pdfFiller, users can easily complete their Cigna Medical Claim Form and other important documents. Whether you need to request reimbursement or provide documentation for insurance purposes, pdfFiller has you covered.