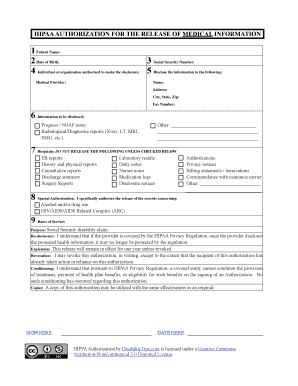
What is soap note mental health?
A SOAP note in mental health refers to a documentation method used by healthcare professionals to record a patient's progress during a therapy session or mental health evaluation. SOAP stands for Subjective, Objective, Assessment, and Plan, and it provides a structured format for organizing information related to the patient's symptoms, observations, diagnosis, and treatment plan. By following the SOAP note format, mental health professionals can effectively communicate and track the patient's progress over time.
What are the types of soap note mental health?
There are several types of SOAP notes commonly used in mental health settings, each serving a specific purpose:
Initial Evaluation Notes: These notes are created during the initial assessment of a patient's mental health condition. They include information about the patient's background, presenting issues, and initial impressions.
Progress Notes: Progress notes are regularly updated as the patient progresses through therapy. They document the patient's current symptoms, improvements, setbacks, and treatment interventions.
Group Therapy Notes: When conducting therapy sessions in a group setting, therapists may use SOAP notes to capture both individual and group observations, discussions, and outcomes.
Crisis Notes: In emergency situations or during a crisis intervention, mental health professionals may use crisis SOAP notes to record critical information about the patient's mental state, interventions, and outcome.
Discharge Summary Notes: These notes summarize the patient's progress, treatment outcomes, and future recommendations upon their discharge from therapy or mental health services.
How to complete soap note mental health
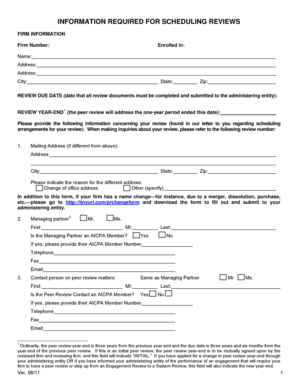
Completing a SOAP note in mental health involves a systematic approach to gathering and documenting information. Here are the steps to follow:
01
Subjective: Begin by collecting subjective information from the patient regarding their symptoms, feelings, concerns, and any recent changes in their mental state.
02
Objective: Observe and record objective information, such as the patient's behavior, appearance, speech, and any observable indicators of distress or improvement.
03
Assessment: Analyze the subjective and objective data to form an assessment of the patient's mental health status. This may include evaluating their symptoms, diagnosing any mental disorders, and identifying any potential risk factors.
04
Plan: Develop a plan of action based on the assessment. This may involve outlining treatment goals, recommending therapeutic interventions, prescribing medication if necessary, and providing support resources.
05
Documentation: Accurately document all relevant information in a clear and concise manner, adhering to the SOAP note format. Use appropriate medical terminology and avoid subjective opinions or biases.
06
Review and Update: Regularly review and update SOAP notes to ensure they reflect the patient's progress accurately. This allows for continuity of care and helps track changes over time.
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.