Soap Note Physical Therapy
What is soap note physical therapy?
SOAP note, which stands for Subjective, Objective, Assessment, and Plan, is a method used by physical therapists to document their patients' progress and treatment plans. It allows therapists to effectively communicate with other healthcare providers and provides a comprehensive overview of the patient's condition.
What are the types of soap note physical therapy?
There are several types of SOAP notes used in physical therapy. These include: 1. Initial Evaluation SOAP Note: This note is created during the patient's first visit and includes information about their medical history, current condition, and initial assessment. 2. Progress SOAP Note: This note is used to track the patient's progress throughout their treatment. It includes updates on their condition, any changes in therapy, and goals achieved. 3. Discharge SOAP Note: This note is created when the patient's treatment is completed. It summarizes the patient's progress, the results of the treatment, and any recommendations for further care.
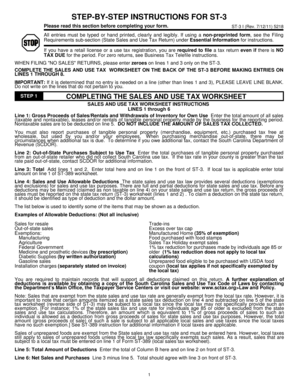
How to complete soap note physical therapy
Completing a SOAP note in physical therapy requires a systematic approach. Here are the steps to follow: 1. Subjective: Begin by documenting the patient's subjective complaints, including their symptoms, pain level, and any relevant medical history. 2. Objective: Record the objective findings of the physical examination, such as range of motion, strength, and any other relevant measurements. 3. Assessment: Based on the subjective and objective information, provide an assessment of the patient's condition, including any diagnoses or treatment goals. 4. Plan: Outline the plan for treatment, including specific interventions, exercises, and any follow-up appointments or referrals. 5. Review and Sign: Review the note for accuracy and completeness, then sign and date it to finalize the documentation.
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.