Get the free Hospital Discharge Summary Report 1992 - 2000 - dhss delaware
Show details
Hospital Discharge Summary Report 1992 2000 January 2002 Delaware Health & Social Services Division of Public Health Bureau of Health Planning and Resources Management Doc. No. 350520020106 ACKNOWLEDGEMENTS
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign
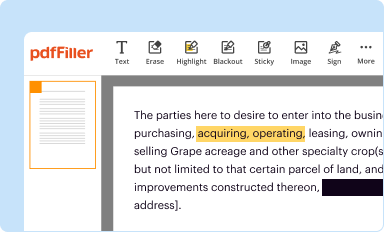
Edit your hospital discharge summary report form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
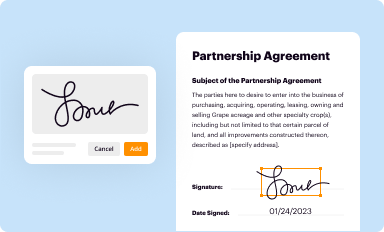
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
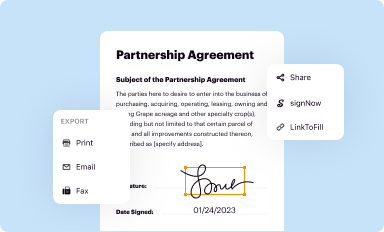
Share your form instantly
Email, fax, or share your hospital discharge summary report form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit hospital discharge summary report online
To use the services of a skilled PDF editor, follow these steps:
1
Set up an account. If you are a new user, click Start Free Trial and establish a profile.
2
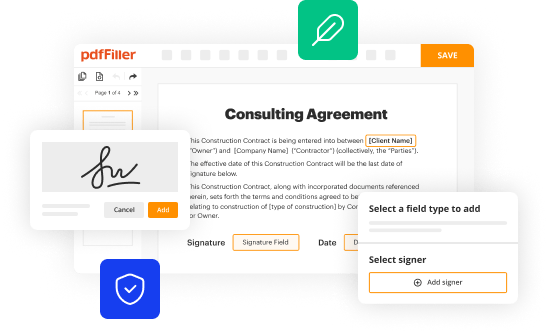
Simply add a document. Select Add New from your Dashboard and import a file into the system by uploading it from your device or importing it via the cloud, online, or internal mail. Then click Begin editing.
3
Edit hospital discharge summary report. Rearrange and rotate pages, add new and changed texts, add new objects, and use other useful tools. When you're done, click Done. You can use the Documents tab to merge, split, lock, or unlock your files.
4
Save your file. Choose it from the list of records. Then, shift the pointer to the right toolbar and select one of the several exporting methods: save it in multiple formats, download it as a PDF, email it, or save it to the cloud.
With pdfFiller, it's always easy to deal with documents. Try it right now
How to fill out hospital discharge summary report
How to fill out a hospital discharge summary report:
01
Start by providing the patient's complete personal information, including their name, address, contact number, and date of birth.
02
Include the admission date and the discharge date to establish the timeline of the patient's hospital stay.
03
Document the reason for admission, whether it was due to an illness, injury, or planned procedure.
04
Outline the diagnoses that were made during the patient's hospital stay. Include any medical conditions or diseases that were identified.
05
Detail the treatments and procedures that were performed, including surgeries, medications administered, and therapies received.
06
Provide a summary of the patient's progress throughout their stay, noting any improvements or complications that arose.
07
Include the instructions for any follow-up care that the patient needs to adhere to after leaving the hospital. This may involve medications to take, therapies to continue, or appointments to schedule.
08
Summarize any discharge recommendations or restrictions, such as dietary restrictions, activity limitations, or lifestyle modifications.
09
Include a list of the healthcare professionals involved in the patient's care during their hospital stay, including their names and specialties.
10
Sign and date the discharge summary report before submitting it to the appropriate department or healthcare provider.
Who needs a hospital discharge summary report?
01
Patients: The primary recipients of a hospital discharge summary report are the patients themselves. It serves as a comprehensive document summarizing their hospital stay, diagnoses, treatments, and instructions for continued care.
02
Primary Care Physicians: The patient's primary care physician needs the hospital discharge summary report to understand the details of the hospitalization, including diagnoses, treatments, and recommended follow-up care, to provide appropriate ongoing care.
03
Specialists: If the patient was under the care of any specialists during their hospital stay, they may also require the discharge summary report to be aware of the treatments and procedures performed and to plan any necessary further interventions.
04
Rehabilitation Centers: In cases where a patient requires ongoing rehabilitation or therapy following their hospital discharge, rehabilitation centers or therapy providers will need the discharge summary report to understand the patient's condition and develop an appropriate treatment plan.
05
Insurance Providers: Insurance providers might request the hospital discharge summary report to assess the medical necessity of the patient's hospitalization and the subsequent ongoing care and procedures.
06
Legal Purposes: In certain legal circumstances, such as medical malpractice claims or disability claims, the hospital discharge summary report may be requested as part of the evidence.
07
Research: Hospital discharge summary reports can be anonymized and used for research purposes to study trends, outcomes, and other healthcare-related topics.
Remember to consult with the appropriate healthcare professionals for specific guidelines and requirements when filling out a hospital discharge summary report.
Fill form : Try Risk Free
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is hospital discharge summary report?
The hospital discharge summary report is a document that outlines the details of a patient's care and treatment during their stay in a hospital, including their diagnosis, treatment plan, and recommendations for follow-up care.
Who is required to file hospital discharge summary report?
Hospital staff, usually the discharging physician or another healthcare provider, is required to file the hospital discharge summary report.
How to fill out hospital discharge summary report?
To fill out a hospital discharge summary report, the healthcare provider must document the patient's medical history, reason for hospitalization, treatment provided, and any follow-up care instructions.
What is the purpose of hospital discharge summary report?
The purpose of the hospital discharge summary report is to provide a comprehensive overview of the patient's hospital stay and treatment to ensure continuity of care during the transition back to the community.
What information must be reported on hospital discharge summary report?
The hospital discharge summary report should include the patient's demographic information, medical history, reason for hospitalization, treatment provided, medications prescribed, and recommendations for follow-up care.
When is the deadline to file hospital discharge summary report in 2024?
The deadline to file the hospital discharge summary report in 2024 is typically within a specified timeframe after the patient's discharge, such as within 30 days.
What is the penalty for the late filing of hospital discharge summary report?
The penalty for the late filing of the hospital discharge summary report may result in fines or potential disciplinary action for the healthcare provider or hospital.
Can I create an electronic signature for signing my hospital discharge summary report in Gmail?
Upload, type, or draw a signature in Gmail with the help of pdfFiller’s add-on. pdfFiller enables you to eSign your hospital discharge summary report and other documents right in your inbox. Register your account in order to save signed documents and your personal signatures.
How do I complete hospital discharge summary report on an iOS device?
Install the pdfFiller app on your iOS device to fill out papers. If you have a subscription to the service, create an account or log in to an existing one. After completing the registration process, upload your hospital discharge summary report. You may now use pdfFiller's advanced features, such as adding fillable fields and eSigning documents, and accessing them from any device, wherever you are.
How do I complete hospital discharge summary report on an Android device?
Use the pdfFiller mobile app to complete your hospital discharge summary report on an Android device. The application makes it possible to perform all needed document management manipulations, like adding, editing, and removing text, signing, annotating, and more. All you need is your smartphone and an internet connection.
Fill out your hospital discharge summary report online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Not the form you were looking for?
Keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.